Drug Addiction: Definition, Types, Causes, Symptoms, Effects, Treatment and Recovery.

Drug addiction, or Substance Use Disorder (SUD), is a chronic condition characterized by the compulsive and harmful use of substances, leading to significant impairment in various areas of life. According to the National Survey on Drug Use and Health, 2021 data, 46.3 million people aged 12 or older (16.5%) had a substance use disorder (SUD) in the past year, including 29.5 million with alcohol use disorder, 24.0 million with drug use disorder, and 7.3 million with both.
Additionally, Ohio recorded its highest number of overdose deaths in 2020, with over 500 fatalities per month according to the 2020 Ohio Drug Overdose Data: General Findings. These statistics highlight the substantial impact of substance use disorders on the population.
The types of drug addiction include alcohol addiction, stimulant addiction, cannabis addiction, opioid addiction, sedative-hypnotic addiction, hallucinogen addiction, and inhalant addiction.
The causes of drug addiction are broadly classified into biological factors, environmental and psychological factors. This includes genetic predisposition, family history, peer influence, mental health condition, social influences, early exposure to substances, and trauma.
The symptoms of drug addiction include cravings, withdrawal symptoms, tolerance, loss of control, neglecting responsibilities, social and interpersonal problems, and continued use despite negative consequences.
The effects of drug addiction include physical health problems, impaired cognitive function, deteriorating relationships, financial difficulties, legal issues, and overall deterioration in quality of life.
Treatment options for drug addiction include a combination of behavioral therapies, medication-assisted treatment, support groups, counseling, and holistic approaches aimed at addressing the physical, psychological, and social aspects of addiction.
What is Drug Addiction?
Drug addiction is recognized as a brain disorder that profoundly affects the reward, motivation, and decision-making systems according to NIDA’s most recent 2024 publication titled Drug Misuse and Addiction. It involves changes in brain chemistry and neural pathways, resulting in a strong and often uncontrollable urge to seek and use substances.
Substance use disorders involve functional changes to brain circuits involved in reward, stress, and self-control on the brain, Goldstein RZ, Volkow ND. 2011 study considers addiction a brain disease that lasts a long time after a person has stopped taking drugs. The persistent nature of drug addiction leads to a cycle of continued drug use despite the negative consequences it brings.
It is diagnosed when an individual’s drug use leads to significant impairment or distress, impacting multiple areas of their life, including physical and mental health, relationships, work, and overall well-being.
According to a 2020 study by the National Institute on Drug Abuse (NIDA), SUD affects approximately 19.7 million adults in the United States, with an estimated 8.5 million individuals suffering from both a substance use disorder and a mental health disorder. It is associated with a range of adverse outcomes, including increased risk of accidents, health problems, legal issues, and social and interpersonal difficulties.
More Resources on Addiction:
Did you know most health insurance plans cover substance use disorder treatment? Check your coverage online now.
What Is The Difference Between Drug Addiction And Drug Dependence?
The key difference between drug addiction and drug dependence lies in their distinct characteristics and impacts on an individual’s life. Drug addiction is characterized by a lack of control over drug use, where individuals continue to use substances despite knowing the harm they cause, indicating significant behavioral and psychological impairment. In contrast, drug dependence is primarily identified by tolerance and withdrawal symptoms, where individuals need larger amounts of a drug to achieve the same effect and experience physical symptoms when drug use is reduced or stopped.
Addiction involves compulsive behavior and a preoccupation with obtaining and using the drug, leading to negative consequences in various areas of life. Dependence occurs without addiction, as individuals develop a dependence on prescribed medications for legitimate medical reasons without exhibiting addictive behaviors. While both conditions coexist, addiction encompasses both physical and psychological components, significantly impairing daily life, whereas dependence reflects the body’s physical adaptation to a substance.
What are the Types of Drug Addiction?
The types of drug addiction are broadly classified into different types which include depressant addiction, opioid addiction, hallucinogen addiction, inhalant addiction, nicotine addiction, sedative-hypnotic addiction, alcohol addiction, and stimulant addiction.
1. Opioid Addiction
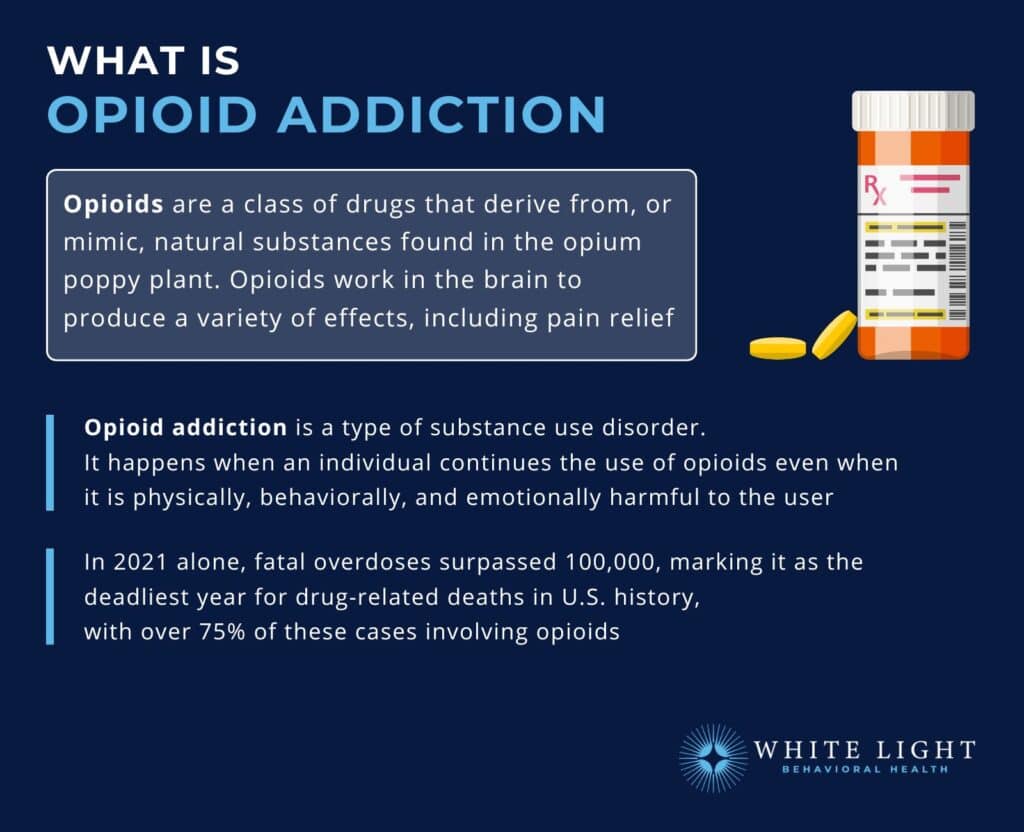
Opioid use disorder (OUD) is defined as the chronic use of opioids that causes clinically significant distress or impairment according to Dydyk AM, Jain NK, Gupta M’s 2024 study on Opioid Use Disorder in StatPearls.
Opioids are a class of drugs that include both legal pain relievers prescribed by doctors, such as Percocet, Tramadol, Oxycodone, hydrocodone, morphine, and fentanyl, Kratom, and illegal drugs like heroin. According to the Centers for Disease Control and Prevention, Over 75% of the nearly 107,000 drug overdose deaths in 2021 involved an opioid.
From 2020 to 2021. Opioids work by binding to opioid receptors in the brain, spinal cord, and other areas of the body, reducing the perception of pain and promoting feelings of euphoria.
In 2016, there were 3,613 opioid-related overdose deaths in Ohio which equates to a rate of 32.9 deaths per 100,000 persons and more than double the national rate of 13.3 deaths per 100,000 according to the National Institute on Drug Abuse (NIDA) Ohio Opioid Summary from 2019.
Symptoms include increased tolerance, severe withdrawal symptoms (e.g., pain, digestive distress, mood swings), uncontrollable cravings, and continued use despite harmful consequences. Causes include chronic pain management, recreational use, genetic predisposition, social environment, and emotional distress.
Individuals with opioid addiction begin using prescription painkillers for legitimate pain but gradually develop tolerance. This tolerance leads to increased usage and eventually drives individuals to illegal opioids, such as heroin, to satisfy cravings.
There are various approaches to rehabilitating and maintaining patients with Opioid Use Disorder (OUD), starting with Medication-assisted treatment (MAT), and cognitive behavioral therapy similar to that used for other chronic conditions.
According to Wakeman, S. E.’s 2020 study, ‘Comparative effectiveness of different treatment pathways for opioid use disorder.’, treatment with buprenorphine or methadone showed significant effectiveness in reducing both overdose risk and serious opioid-related acute care use. The treatment reduced overdose risk by 76% at 3 months and by 59% at 12 months. Similarly, it decreased serious opioid-related acute care use by 42% at 3 months and by 26% at 12 months.
2. Stimulant addiction
Stimulants are substances that increase activity in the body and brain, raising levels of physiological or nervous activity in the CNS. Common stimulants include caffeine, cocaine, methamphetamine, and prescription medications such as Suboxone, Gabapentin, Adderall, Ritalin, and Wellbutrin.
The symptoms of stimulant addiction include heightened alertness, excessive energy, decreased appetite, increased heart rate and blood pressure, insomnia, rapid speech, paranoia, and hallucinations.
Causes include the desire to enhance performance, achieve weight loss, self-medicate for depression or ADHD, and the increase in dopamine levels leading to feelings of pleasure and satisfaction.
The misuse of prescription stimulants, antidepressants, sedatives, steroids, or other drugs during adolescence negatively impacts brain and body development.
An example of stimulant addiction is someone with methamphetamine use disorder enjoying the euphoric rush of using methamphetamines to the point where they will use it despite the physical, mental, and societal consequences.
The Substance Abuse and Mental Health Services Administration (SAMHSA) warns that misusing prescription stimulants, antidepressants, sedatives, or other drugs during adolescence negatively impacts the development of the brain and body.
Treatment for stimulant addiction typically involves behavioral therapies like cognitive-behavioral therapy (CBT) and contingency management, along with support groups and peer counseling. Professional counseling is also essential to address the psychological and emotional issues associated with addiction.
3. Alcohol Use Disorder

Alcohol addiction, also known as alcoholism or Alcohol Use Disorder (AUD), involves a physical and emotional dependency on alcohol.
According to the 2022 National Survey on Drug Use and Health (NSDUH), 29.5 million people ages 12 and older (10.5% in this age group) had AUD in the past year. It is characterized by the inability to manage drinking habits despite negative personal and social consequences.
Symptoms include a strong craving for alcohol, inability to limit drinking, withdrawal symptoms (e.g., shaking, nausea, anxiety), high tolerance, and neglect of responsibilities. The causes of AUD include genetic predisposition, social factors, environmental cues, psychological stress, and co-occurring mental health disorders.
An example of Alcohol Use Disorder is someone who starts drinking to unwind after work but eventually finds themselves needing multiple drinks throughout the day to function normally and continues to drink despite the troubles it causes at home and professionally.
Treatment for alcohol use disorder typically involves a combination of detoxification under medical supervision, behavioral counseling, and therapy. Support groups like Alcoholics Anonymous (AA) play a crucial role in providing peer support and accountability.
Cognitive-behavioral therapy (CBT) is particularly effective; According to Carroll, K. M., & Kiluk, B. D.’s 2017 study, ‘Cognitive behavioral interventions for alcohol and drug use disorders: Through the stage model and back again.’, published in the Psychology of Addictive Behaviors reports that at least 58% of those who receive CBT for alcohol use disorder treatment fare better than their counterparts who do not. Medications such as disulfiram, naltrexone, and acamprosate serve to reduce the desire to drink, manage withdrawal symptoms, and prevent relapse. These medications play a significant role in the treatment of alcohol use disorder.
Contact us today to schedule an initial assessment or to learn more about our services. Whether you are seeking intensive outpatient care or simply need guidance on your mental health journey, we are here to help.
4. Hallucinogenic addiction
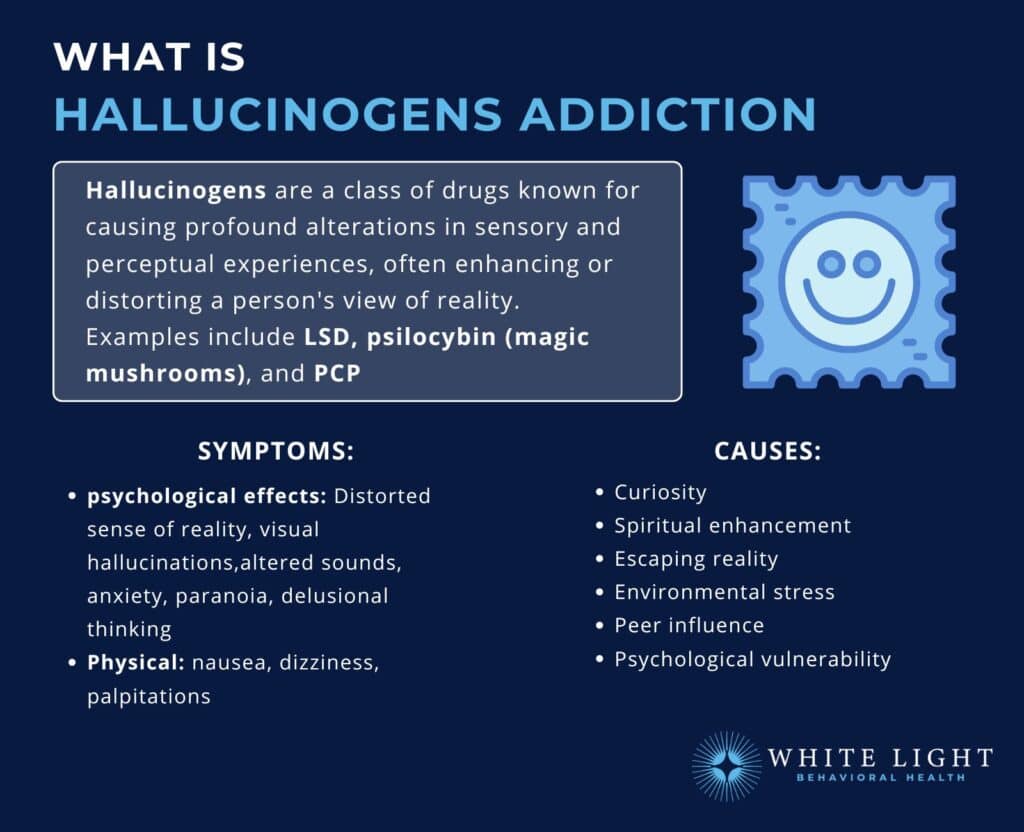
Hallucinogens are a class of drugs known for causing profound alterations in sensory and perceptual experiences, often enhancing or distorting a person’s view of reality. Common hallucinogens include LSD, psilocybin (magic mushrooms), and PCP (phencyclidine), as well as ketamine, which also has dissociative effects.
According to Salas-Wright, C. P.’s 2021 study, ‘Driving while under the influence of hallucinogens: Prevalence, correlates, and risk profiles.’, 2.42% of the U.S. population used hallucinogens, with 0.21% driving under their influence. Among hallucinogen users specifically, 8.94% reported driving while under the influence at least once in the past year, raising significant safety concerns as these substances affect perception and risk-taking behavior.
Symptoms include distorted reality, visual hallucinations, altered sounds, anxiety, paranoia, delusional thinking, nausea, dizziness, and palpitations. Causes include curiosity-driven experimentation, the desire to enhance spiritual experiences, escape from reality, and psychological dependence due to stress or peer influence.
Hallucinogen use is typically experimental and less common than other forms of drug use, but its impact on mental health is significant.
A person experimenting with LSD might initially use it out of curiosity but eventually find themselves using it frequently to escape reality, leading to psychological dependence where they use the drug despite its negative consequences. It’s important to note that hallucinogens do not cause physical dependence and instead cause psychological dependence so there are no medications to help with the physical aspect of hallucinogen addiction recovery.
Treatment for hallucinogen addiction typically includes psychotherapy to address and change drug-taking behaviors, support groups for ongoing support and understanding, and education about the risks associated with drug use to promote informed decisions.
6. Nicotine Addiction
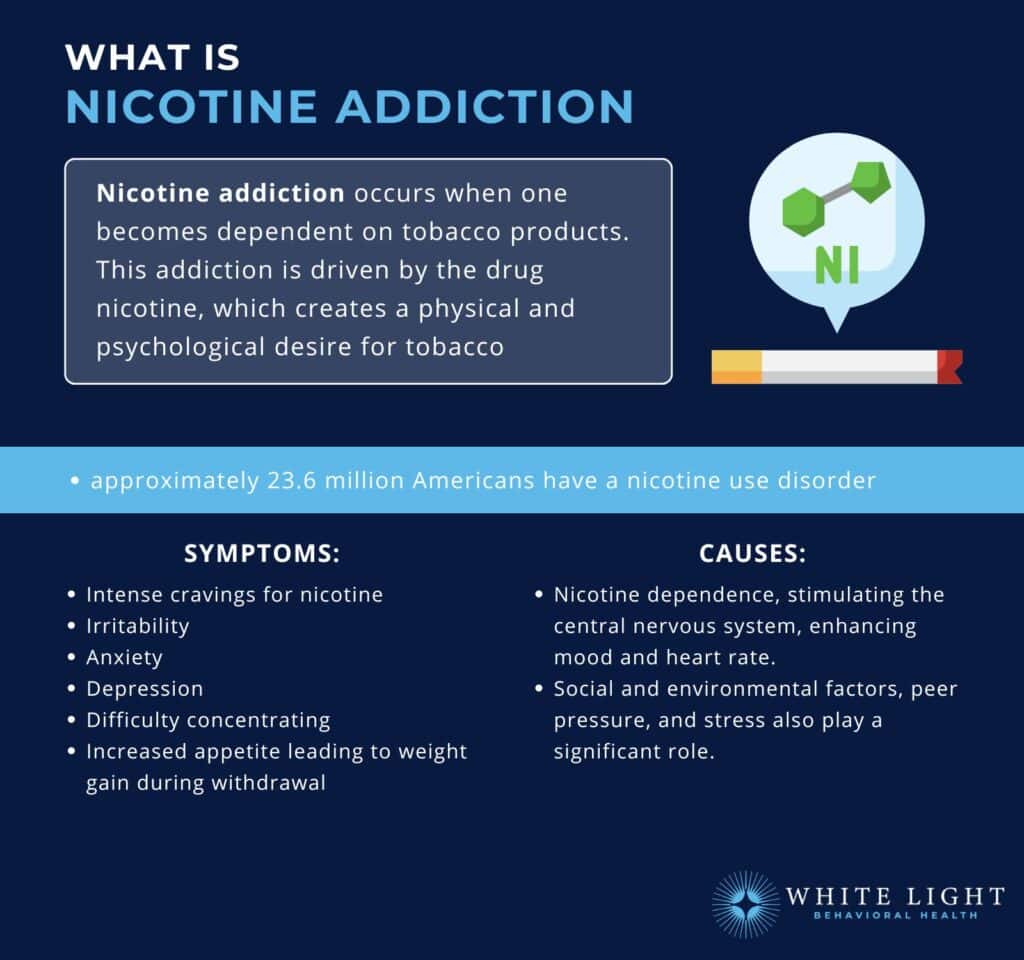
Nicotine addiction is the compulsive use of tobacco products despite the harmful health consequences.
Nicotine, an addictive chemical found in tobacco, quickly stimulates the brain and is considered as addictive as heroin or cocaine.
According to the National Survey on Drug Use and Health, in 2021, among people aged 12 or older, 22.0% (or about 61.6 million people) reported using tobacco products or vaping nicotine in the past 30 days, 15.6% (or about 43.6 million people) reported smoking cigarettes in the past 30 days, and 4.7% (or about 13.2 million people) reported vaping nicotine in the past 30 days.
Symptoms include strong cravings, irritability, anxiety, depression, and difficulty concentrating when trying to quit, along with physical symptoms like increased appetite and weight gain. Causes include the mood-altering effects of nicotine, genetic factors, social environment, and stress.
Someone addicted to nicotine might start smoking socially but soon find themselves needing a cigarette to handle stress, leading to a daily habit that becomes difficult to break.
Treatment options for Tobacco and nicotine addiction are listed below:
- Nicotine replacement therapies (NRTs) like patches, gum, lozenges, inhalers, or nasal sprays to reduce withdrawal symptoms and smoking urges.
- Non-nicotine medications such as bupropion and varenicline to reduce cravings and withdrawal symptoms.
- Behavioral therapies and support groups to assist individuals in quitting smoking.
8. Inhalant Addiction
Inhalant addiction involves the repeated inhaling of vapors from household or industrial chemicals to achieve a euphoric effect. Commonly abused inhalants include solvents, aerosols, gases, and nitrites, known colloquially as ‘huffing,’ with examples such as ether, glue, and paint thinner.
Symptoms include dizziness, euphoria, lethargy, slurred speech, lack of coordination, and irritability. Long-term abuse leads to neurological damage and impaired cognitive function. Causes include easy accessibility, low cost, rapid onset of euphoria, peer pressure, and stress.
Inhalant use is more prevalent among adolescents, with significant risks for long-term brain damage. An example of inhalant abuse is a teenager who might start inhaling household chemicals out of curiosity or peer pressure but soon become addicted due to the quick and intense high they provide, leading to repeated use and serious health consequences.
According to Lipari, R. N. ‘s 2017 study, ‘Understanding adolescent inhalant use’, approximately 684,000 adolescents aged 12 to 17 used inhalants in 2015. The study found that adolescents were more likely than adults to use inhalants (2.7% vs 0.4%), with female adolescents showing higher rates than males (3.2% vs 2.3%). Most users (59%) reported using inhalants 1-11 days in the past year, with felt-tip pens/markers being the most commonly used substance.
Treatment for inhalant addiction involves detoxification, supportive care for withdrawal symptoms, comprehensive behavioral interventions, and counseling to address psychological aspects and prevent relapse.
9. Depressant Addiction

Depressants are a class of drugs that reduce arousal and stimulation in the user, affecting the central nervous system (CNS) by slowing down brain function and enhancing the production of a neurotransmitter called gamma-aminobutyric acid (GABA).
According to the National Institute on Drug Abuse 2022 report, ‘Benzodiazepines and opioids’, In 2021, nearly 14% of overdose deaths involving opioids also involved benzodiazepines, a type of prescription sedative commonly prescribed for anxiety or to help with insomnia.
Common depressants include alcohol, benzodiazepines (like Valium and Xanax), barbiturates, and other substances such as Ambien, clobazam, eszopiclone, NyQuil, and gamma hydroxybutyrate (GHB).
Benzodiazepines and sedative-hypnotics both fall under the broader category of depressants, which are substances that slow down brain activity. However, there are some distinctions between these terms based on their primary use and effects.
Symptoms of depressant addiction include slurred speech, confusion, disorientation, lowered blood pressure, respiratory depression, decreased motor coordination, and severe withdrawal symptoms. Addiction is often driven by a combination of genetic, environmental, and psychological factors, with individuals using depressants for their calming effects, especially those with underlying mental health issues.
What Are The Most Common Benzodiazepine Addictions?
The Most Common Benzodiazepine Addictions include Alprazolam (Xanax), Diazepam (Valium), Lorazepam (Ativan), and Clonazepam (Klonopin). These widely prescribed medications are followed by Chlordiazepoxide (Librium), Temazepam (Restoril), and Oxazepam (Serax) in terms of addiction frequency.
Here is a list of some of the most commonly abused benzodiazepines:
- Alprazolam (Xanax): Commonly prescribed for anxiety and panic disorders, it has a high potential for abuse and addiction due to its fast-acting effects. Xanax addiction has severe withdrawal symptoms.
- Diazepam (Valium): Used for anxiety, muscle spasms, and seizures, it is another benzodiazepine with a significant potential for addiction.
- Lorazepam (Ativan): Prescribed for anxiety and used as a sedative before surgeries, it is known for its potential for dependence and abuse.
- Clonazepam (Klonopin): Used to treat seizures and panic disorders, it has a longer half-life, which contributes to clonazepam dependence and addiction.
- Chlordiazepoxide (Librium): Often prescribed for anxiety and alcohol withdrawal symptoms, it also carries a risk of addiction.
- Temazepam (Restoril): Commonly used as a sleep aid, it leads to dependency and abuse when used for extended periods.
- Oxazepam (Serax): Used for anxiety and alcohol withdrawal, it is less commonly abused than some other benzodiazepines but still carries a risk of addiction.
These medications, while effective for intended medical purposes, lead to tolerance, physical dependence, and addiction if misused or taken for extended periods. Misuse of these medications poses significant risks to individuals’ health and well-being.
What are the Symptoms of Drug Addiction?
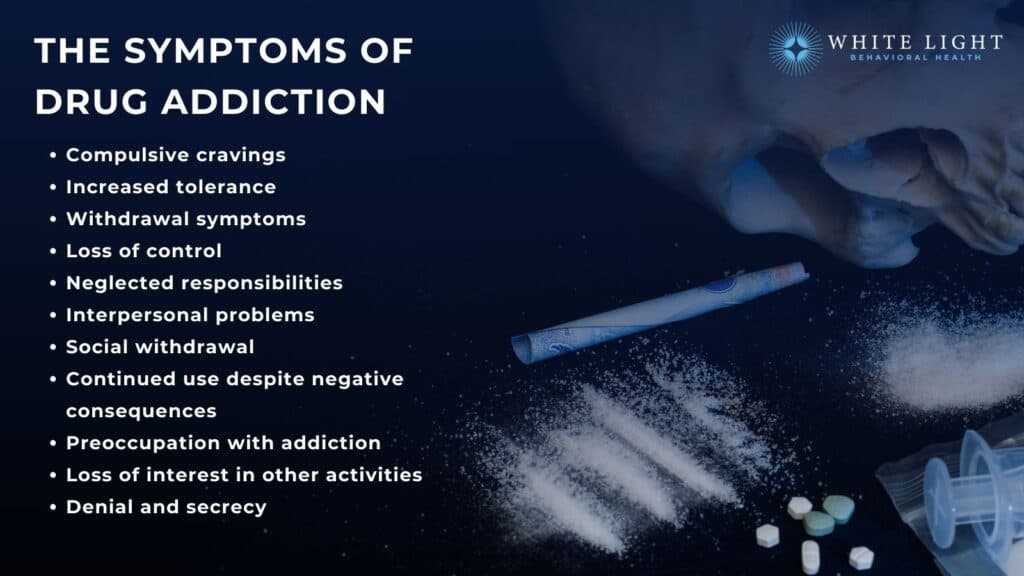
The symptoms of drug addiction range from compulsive cravings to tolerance, loss of control, social withdrawal, neglected responsibilities, and continued use despite negative consequences.
Here are some common symptoms that indicate the presence of addiction:
- Compulsive cravings: Strong and persistent urges or cravings to engage in the use of drugs, often leading to a loss of control over consumption or engagement.
- Increased tolerance: Needing larger amounts of the substance or engaging in more intense behaviors to achieve the desired effect or experiencing diminished effects with continued use. According to recent facts about tolerance from CDC, almost 50% of drug overdose deaths involved the use of multiple drugs.
Additionally, tolerance to a particular drug also increases to other drugs in the same class.This is known as cross-tolerance.
- Withdrawal symptoms: Experiencing physical or psychological symptoms when attempting to stop or reduce substance use or engagement in addictive behaviors.
These symptoms include anxiety, irritability, restlessness, nausea, sweating, insomnia, and depression. - Loss of control: Difficulty limiting or controlling the frequency, duration, or amount of substance use or engagement in addictive behaviors, despite repeated unsuccessful attempts to quit or cut back.
- Neglected responsibilities: Neglecting or abandoning previously important responsibilities at work, school, or home due to preoccupation with the addictive substance or behavior.
- Interpersonal problems: Experiencing conflicts or strained relationships with family members, friends, or colleagues due to the consequences of addiction, such as lying, stealing, or engaging in risky behaviors.
- Social withdrawal: Withdrawing from social activities, hobbies, or interests previously enjoyed in favor of substance use.
- Continued use despite negative consequences: Persisting in using the substance even when aware of the adverse physical, psychological, social, or financial consequences associated with them.
- Preoccupation with addiction: Spending a significant amount of time thinking about obtaining, using, or recovering from the substance.
- Loss of interest in other activities: Showing a diminished interest in previously enjoyable activities or hobbies that are unrelated to the addiction.
- Denial and secrecy: Denying or minimizing the severity of the addiction when confronted by others, and engaging in secretive behaviors to hide the extent of substance use or engagement in addictive behaviors.
Rediscover Life at White Light Behavioral Health
Get the compassionate support you deserve. We're here to help you reclaim joy, wellness, and a brighter future.
Our Facility
What are the Causes of Drug Addiction?
The causes of drug addiction are categorized into biological, psychological, social, and environmental influences. Here are some key causes of addiction:
What Are The Biological Causes Of Drug Addiction?
The biological causes of drug addiction include genetic predisposition, brain chemistry and co-occurring mental health disorders:
- Genetic factors: Genetic predisposition plays a role in addiction susceptibility, as certain individuals inherit a higher vulnerability to developing addictive behaviors. According to the National Institute on Drug Abuse, genetics account for 40% – 60% of addiction risk.
- Brain chemistry and physiology: Drug addiction involves alterations in brain chemistry, particularly in the reward and pleasure centers of the brain.
These changes create a heightened response to substances or behaviors, reinforcing the cycle of addiction. - Co-occurring mental health disorders: Individuals with underlying mental health conditions, such as depression, anxiety, or trauma-related disorders, will turn to substances or behaviors as a means of self-medication, leading to addiction.
What are the Environmental Causes of Drug Addiction?
The environmental causes of drug addiction include unstable home environments, peer pressure in schools or neighborhoods, and traumatic life experiences. These risk factors, along with easy access to substances and poor social support systems trigger addictive behaviors.
Here are the key environmental causes of drug addiction:
- Availability and accessibility: The availability and ease of access to substances play a significant role in the initiation and progression of addiction.
- Early-life experiences: Adverse childhood experiences, including neglect, abuse, trauma, or unstable family environments increase the likelihood of developing addiction later in life, as individuals seek substances or behaviors to cope with emotional pain or stress.
What are the Social and Cultural Causes of Drug Addiction?
Social and cultural factors play significant roles in causing drug addiction. Peer pressure, family dynamics, and community attitudes directly influence how people view and use drugs.
Cultural practices, social acceptance of certain substances, and environmental stressors normalize drug use and increase addiction risks. Additionally, societal norms around substance use, especially in entertainment and media, often shape individual behaviors and choices regarding drug experimentation and continued use.
What are the Psychological Factors that Cause Addiction?
The psychological factors that cause addiction include specific vulnerabilities like low self-esteem, impulsivity, sensation-seeking tendencies, and poor coping skills. These psychological factors directly contribute to how addiction develops and takes hold. Understanding these factors is important because addiction’s causes are complex and multifaceted, with different combinations of factors affecting each person uniquely.
Are you covered for treatment?
White Light Behavioral Health is an approved provider for Blue Cross Blue Shield and TUFTS, while also accepting many other major insurance carriers.
Check Coverage Now!What are the 6 Stages of Drug Addiction?
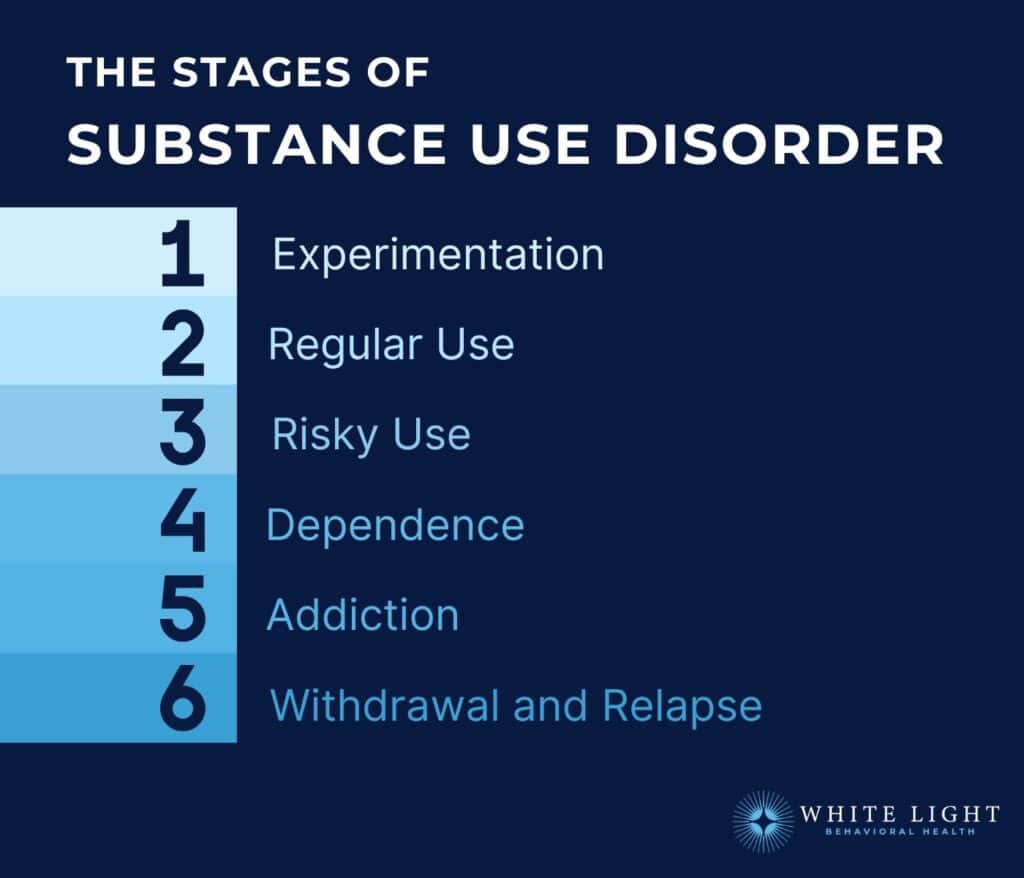
The 6 Stages of Drug Addiction include initial experimentation with substances, progression to regular usage patterns, escalation to risky behavior, development of dependence, establishment of addiction, and experiences with withdrawal and relapse. These stages represent critical transitions from casual exposure to compulsive drug use, marked by increasing tolerance, loss of control, and significant life impacts.
Here are the 6 stages of drug addiction in detail below:
1. Experimentation: This stage involves initial exposure to substances, driven by curiosity, peer influence, or a desire for new experiences. It involves trying substances infrequently or in social settings.
2. Regular Use: In this stage, drug use becomes more frequent and begins to serve a purpose, such as coping with stress, enhancing mood, or escaping from problems. Individuals still believe they have control over their substance use.
3. Risky Use: Drug use escalates, and individuals engage in more frequent and higher doses of drugs. They start taking risks, such as driving under the influence or engaging in unsafe behaviors while using.
4. Dependence: Dependence is characterized by the body and brain becoming accustomed to the presence of the substance.
Physical and psychological dependence develops, leading to withdrawal symptoms when substance use is reduced or stopped. Cravings and a loss of control over substance use become more pronounced.
According to Lopez-Quintero, C.’s 2011 study, ‘Probability and predictors of transition from first use to dependence on nicotine, alcohol, cannabis, and cocaine: results of the National Epidemiologic Survey on Alcohol and Related Conditions (NESARC).’, nicotine shows the highest probability of dependence at 67.5%, meaning more than two-thirds of smokers will become dependent.
Alcohol and cocaine have similar rates at 22.7% and 20.9% respectively, while cannabis shows the lowest at 8.9%. Interestingly, despite nicotine’s high dependence rate, it takes the longest to develop (27 years), while cocaine and cannabis lead to dependence much faster (4-5 years).
5. Addiction: At this stage, individuals experience a compulsive need to use drugs despite negative consequences.
Drug use becomes the primary focus of their lives, often at the expense of relationships, work, and personal well-being. Efforts to quit or cut down on drug use are usually unsuccessful.
6. Withdrawal and Relapse: When individuals attempt to stop or reduce drug use, they experience withdrawal symptoms that cause physical and psychological distress.
Withdrawal symptoms significantly impact the individual’s overall well-being and complicate the recovery process. The risk of relapse is high during this stage, as individuals turn back to drug use to alleviate withdrawal symptoms or cope with cravings.
According to the FDA’s 2023 research initiative on opioid use disorder (OUD), relapse rates among individuals with OUD are alarmingly high, ranging from 65-70%, highlighting the significant challenges in maintaining long-term recovery.
Not everyone linearly progresses through these stages, and individuals enter treatment or seek help at any stage. Early intervention and treatment interrupt the progression of drug addiction and increase the likelihood of successful recovery.
What are the Treatment Options for Drug Addiction?

The Treatment Options for Drug Addiction include medically-supervised detoxification, comprehensive rehabilitation programs, and evidence-based therapeutic interventions. Various approaches like behavioral counseling, medication assistance, and holistic treatments work together to support recovery and healing.
According to NIDA (2020), effective treatment must address all aspects of addiction, not just substance use, to improve recovery outcomes and reduce the likelihood of relapse. Here’s a list of the treatment options used for addiction.
- Detoxification (Detox): Detoxification is often the first step in addiction treatment, primarily for substance addictions. It involves the supervised withdrawal from addictive substances in a safe and supportive environment, with medical assistance to manage withdrawal symptoms.
- Inpatient Rehabilitation: Inpatient or residential rehabilitation programs provide intensive, 24/7 care in a structured environment.
They offer a range of therapies, counseling, support groups, and holistic approaches to address the physical, psychological, and social aspects of addiction.
- Outpatient Rehabilitation: Outpatient programs allow individuals to receive treatment while living at home. They offer flexibility in scheduling and are suitable for individuals with a strong support system and a lower risk of relapse.
Outpatient programs include individual and group counseling, therapy sessions, and support group participation.
- Medication-Assisted Treatment (MAT): MAT combines medications with behavioral therapies to treat substance addictions. Medications help manage withdrawal symptoms, reduce cravings, and normalize brain chemistry.
This approach is commonly used for opioid and alcohol addictions.
- Cognitive-behavioral therapy (CBT): CBT is a widely used therapeutic approach that helps individuals identify and change negative thought patterns and behaviors associated with addiction. It focuses on developing coping strategies, enhancing problem-solving skills, and preventing relapse.
- Motivational Interviewing (MI): MI is a counseling technique that helps individuals explore and resolve their ambivalence about changing addictive behaviors.
It aims to enhance motivation and commitment to recovery by addressing underlying motivations and concerns.
- 12-Step Programs: 12-Step Programs are structured recovery programs, such as Alcoholics Anonymous (AA) and Narcotics Anonymous (NA), that provide peer support and a framework for recovery through group meetings, mentorship, and the process of working through the 12 steps of recovery.
- Holistic Approaches: Holistic interventions, such as yoga, meditation, art therapy, and mindfulness practices, complement traditional treatment methods. These interventions promote self-awareness, reduce stress, facilitate emotional healing, and enhance overall well-being.
- Family Therapy: Family therapy involves the participation of family members in the treatment process.
It aims to improve communication, address dysfunctional dynamics, and provide support and education for both the individual with addiction and their loved ones.
- Aftercare and Continuing Support: After completing a formal treatment program, individuals benefit from ongoing support and aftercare services. This includes outpatient counseling, support groups, sober living environments, and relapse prevention strategies.
How Does Drug Addiction Affect Family Dynamics?
Drug addiction significantly impacts family dynamics, often creating a stressful and sometimes volatile environment.
Families experience increased conflict, mistrust, and emotional distress as they cope with a loved one’s addictive behaviors.
Financial difficulties are also common, as resources are diverted towards sustaining the addiction or dealing with legal troubles. In terms of emotional effects, family members often feel a range of emotions from guilt and shame to anger and fear.
Family therapy is frequently recommended as part of the treatment process to address these issues, heal relationships, and improve communication and coping strategies.
What Are The Different Types of Addiction?
Addiction is broadly categorized into physical (substance) addiction and behavioral (process) addiction.
Physical (Drug) Addiction
Physical addiction involves the dependence on substances such as drugs or alcohol. This type of addiction is characterized by the body’s adaptation to the substance, leading to tolerance and withdrawal symptoms when the substance is not used.
Examples:
- Alcohol Addiction: Dependence on alcoholic beverages, leads to health issues and impaired social functioning.
- Drug Addiction: Includes addiction to both prescription and illegal drugs, such as opioids, crack cocaine, methamphetamine, and cannabis.
- Nicotine Addiction: Dependence on tobacco products, leading to health risks like lung cancer and heart disease.
Characteristics:
- Tolerance: Needing more of the substance to achieve the same effect.
- Withdrawal Symptoms: Physical and mental symptoms that occur when reducing or stopping the substance.
Did you know most health insurance plans cover substance use disorder treatment? Check your coverage online now.
Behavioral (Process) Addiction
Behavioral addiction, also known as process addiction, involves the compulsive engagement in rewarding non-substance-related behaviors despite negative consequences. These addictions are as debilitating as physical addictions.
Examples:
- Gambling Addiction: Compulsive gambling behavior that disrupts personal and professional life.
- Internet and Gaming Addiction: Excessive use of the internet or video games that interferes with daily responsibilities and relationships.
- Sex Addiction: Compulsive engagement in sexual activities, often leading to significant personal distress and relationship problems.
- Shopping Addiction: Compulsive buying behavior that results in financial and personal problems.
- Food Addiction: Compulsive eating behavior is linked with emotional regulation issues and health consequences.
Characteristics:
- Compulsive Behavior: Engaging in the behavior despite understanding its negative impact.
- Cravings and Obsession: Persistent thoughts and urges to engage in the behavior.
Impulse Control Disorders
Impulse control disorders are characterized by the inability to resist a temptation or urge that harms oneself or others. While they share similarities with behavioral addictions, they are often classified separately due to their distinct features.
Examples:
- Kleptomania: Compulsive stealing.
- Pyromania: Compulsive urge to start fires.
- Intermittent Explosive Disorder: Recurrent aggressive outbursts.
Characteristics:
- Lack of Control: Inability to resist impulses, leading to harmful actions.
- Tension and Relief Cycle: A buildup of tension before the act, followed by a sense of relief after.
Understanding the different types of addiction is crucial for effective treatment and support. Physical addictions involve substance dependence, leading to tolerance and withdrawal symptoms.
Are There Cultural Differences In The Perception And Treatment Of Drug Addiction?
Yes, there are cultural differences in the perception and treatment of drug addiction. According to the National Institute on Drug Abuse (NIDA, 2019), cultural factors significantly influence how drug addiction is perceived, stigmatized, and treated across different societies. Understanding these cultural nuances is vital for developing effective and culturally sensitive addiction interventions.
How Many People Recover from Drug Addiction?
People recover from drug addiction at varying rates. According to the National Institute on Drug Abuse (NIDA) recovery rates will range between 40-60% for those receiving treatment. Long-term success, defined by sustained recovery, is seen in approximately 25-50% or more of individuals who actively engage in comprehensive treatment programs and utilize relapse prevention strategies.
What Is The Impact Of Drug Addiction On The Brain?
Drug addiction impacts the brain in several fundamental ways, primarily by changing its structure and functioning. When addictive substances enter the system, they disrupt the brain’s neurotransmitter networks, which are essential for neural communication. These disruptions specifically target areas controlling reward, motivation, learning, and memory processes.
As addiction progresses, it weakens the brain circuits responsible for impulse control, making drug resistance increasingly challenging for the affected individual. The lasting impact extends beyond drug-seeking behavior, affecting both cognitive abilities and emotional control, which results in permanent brain damage.
Contact us today to schedule an initial assessment or to learn more about our services. Whether you are seeking intensive outpatient care or simply need guidance on your mental health journey, we are here to help.
What Role Do Neurotransmitters Play In Drug Addiction?
Neurotransmitters such as dopamine and serotonin play essential roles in the development and continuation of drug addiction. Drugs often mimic or enhance the actions of neurotransmitters, leading to altered mood, behavior, and perceptions.
For instance, stimulants like cocaine increase dopamine levels quickly, which significantly affects the brain’s reward system, reinforcing drug use as a pleasurable habit. Over time, these drugs alter brain chemistry and circuitry, leading to dependency and addiction.
Share This Post
















