Drug Tolerance: Causes, Impacts, Assessment, Consequences, and Management
Drug tolerance develops when an individual requires higher doses of a substance to achieve the same effect due to neural adaptation. Unlike drug resistance, which involves a failure to respond to a therapeutic drug, tolerance differs fundamentally from drug dependence and addiction, which are characterized by compulsive use and withdrawal symptoms.
Tolerance is a physical phenomenon that precedes these more complex conditions but is distinct in its scope and progression. Half of Americans aged 12 and older have used illicit drugs, contributing to nearly 1 million overdose deaths since 2000, with $35 billion allocated to drug control in 2020, underscoring the prevalence and societal cost of drug tolerance and addiction, according to the National Center for Drug Abuse Statistics (NCDAS).
The primary causes of drug tolerance include genetic predispositions, receptor activity changes, and frequent drug use, all of which contribute to the gradual reduction in the drug’s effectiveness. Mechanistically, tolerance involves either metabolic tolerance, where the body processes the drug more efficiently, or cellular tolerance, involving adaptations in the brain’s receptors. Both processes reduce the drug’s potency over time.
Drug tolerance has profound implications, including the need for increased dosages, heightened risk of side effects, and potential overdose. As drug tolerance increases, individuals require higher doses to achieve the same effect, raising the risk of overdose.
In 2022, the CDC reported 107,941 drug overdose deaths in the U.S., with an age-adjusted rate of 32.6 per 100,000 population. It also exacerbates dependency risks and complicates addiction recovery.
Understanding these risks is important for developing effective treatment strategies, particularly in cases involving opioids, sedatives, and other high-risk substances.
Assessment of drug tolerance involves clinical evaluations, patient history analysis, and diagnostic tools such as structured questionnaires and drug-level monitoring. These methods help determine the severity of tolerance and guide tailored interventions to manage its impact effectively. Tools like the Drug Abuse Screening Test (DAST) and CAGE questionnaire, authorized by organizations like the Substance Abuse and Mental Health Services Administration (SAMHSA) and the American Society of Addiction Medicine (ASAM), are commonly used for self-assessment, while urine tests or blood levels of specific substances are used to assess drug levels.
Short-term consequences of drug tolerance include diminished therapeutic effects and escalated dosage needs, while long-term effects lead to dependency, withdrawal, and even cognitive or physical deterioration. These consequences underline the importance of addressing tolerance promptly in both clinical and personal contexts.
Effective management strategies for drug tolerance focus on dose management, periodic drug holidays, and behavioral therapies like CBT and motivational interviewing. Around 40-60% of individuals in addiction treatment experience positive outcomes, as reported by the National Institute on Drug Abuse (NIDA) and the Substance Abuse and Mental Health Services Administration (SAMHSA). Preventive measures, such as regular monitoring and exploring non-drug alternatives, are equally important for mitigating tolerance risks and promoting sustainable recovery.
More Resources on Addiction:
What is Drug Tolerance?
Drug tolerance is a physiological state in which an individual requires an increased dose of a drug to achieve the same effect previously attained with a lower dose. Drug tolerance occurs when the body becomes less responsive to a substance after repeated exposure.
Over time, an individual needs higher doses of the drug to achieve the same effect as the body adapts to the presence of the substance. The reduced response results from various physiological changes, including alterations in receptor activity or changes in the drug’s metabolism, according to the MSD Manual in “Tolerance and Resistance to Drugs.”
Tolerance develops to both the desired effects (e.g., pain relief or euphoria) and the side effects (e.g., sedation or nausea). Tolerance significantly impacts the development of substance dependence as individuals increase their use to overcome tolerance, raising the risk of addiction. Repeated use of substances like alcohol, opioids, and stimulants leads to varying degrees of tolerance, depending on the drug and the individual’s physiology.
Did you know most health insurance plans cover substance use disorder treatment? Check your coverage online now.
Why Does Drug Tolerance Matter?
Drug tolerance matters because it influences both treatment outcomes and the risk of relapse, as studied by Healthline in “Understanding Drug Tolerance.” As individuals develop tolerance, they require higher doses of a substance to achieve the same effect, increasing physical dependence and complicating withdrawal. This reduced response to drugs also poses challenges for treatment, as medications used in detoxification or maintenance therapy need careful adjustment to be effective without fostering new dependencies.
Furthermore, tolerance contributes to relapse risk after a period of abstinence, according to the Alcohol and Drug Foundation. Individuals lose their tolerance but resume drug use at previously high doses, which leads to overdose.
Understanding and addressing drug tolerance is important for designing effective, individualized rehab programs that prioritize safety and long-term recovery. It is important to make gradual dose adjustments and seek therapies like cognitive-behavioral therapy to manage tolerance-related challenges during rehabilitation.
How Does Drug Tolerance Differ from Drug Resistance?
Drug tolerance differs from drug resistance in its mechanisms and implications. Drug tolerance refers to the reduced effects of a substance with repeated exposure, requiring higher doses to achieve the same result. It is common with psychoactive drugs like opioids or alcohol.
In contrast, drug resistance involves the complete failure to respond to a drug, according to the World Health Organization (WHO). This is seen in medical treatments like antibiotics or cancer therapies, where microorganisms or cells adapt and neutralize the drug’s effectiveness. While tolerance is linked to changes in the nervous system’s response, resistance is a biological adaptation at a cellular level, posing different challenges in medical and therapeutic contexts.
What Causes Drug Tolerance to Develop?
The causes of drug tolerance include genetic factors, frequency of use, and physiological adaptations. These factors interact to influence how quickly and to what extent tolerance develops, varying widely among individuals.
The frequency of opioid and benzodiazepine use for medical purposes significantly contributes to drug tolerance issues. According to the CDC, opioid prescriptions have steadily increased, with over 191 million opioid prescriptions dispensed in 2020, and benzodiazepines are prescribed in about 66 million office visits annually, which exacerbates tolerance concerns.
As these medications are used frequently for chronic pain management and anxiety disorders, the body builds tolerance, requiring higher doses to achieve the same therapeutic effects, which increases the risk of dependence and overdose.
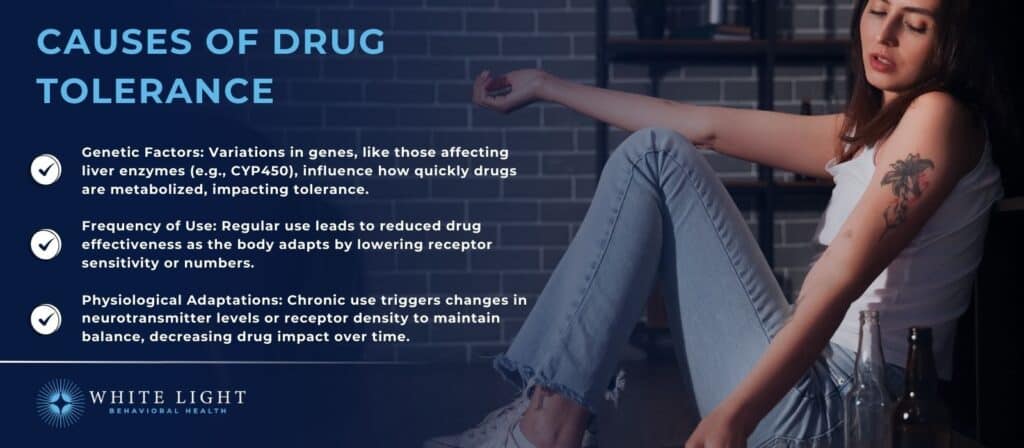
The causes of drug tolerance are as follows:
- Genetic Factors: Genetic predisposition affects how enzymes metabolize drugs and how neurotransmitter systems adapt to substances. For instance, variations in liver enzymes like CYP450 influence the rate of drug breakdown, leading to faster tolerance in some individuals, according to the Mayo Clinic.
- Frequency of Use: Repeated exposure to a substance triggers reduced response over time, as studied by Pietrzykowski AZ, Treistman SN. et al. 2008, in “The molecular basis of tolerance.” The body or brain adapts by decreasing receptor sensitivity or reducing the number of active receptors, particularly in the case of drugs like opioids or benzodiazepines.
- Physiological Adaptations: Homeostatic processes in the body work to maintain balance.
Chronic drug use alters neurotransmitter levels or receptor density, making the drug less effective over time, according to a study by Davis S, Zhu J. et al. 2022, titled “Substance abuse and neurotransmission.” This is particularly common in substances that affect the central nervous system, like alcohol or stimulants.
How Does the Brain Build Tolerance?
The brain builds tolerance through receptor desensitization and changes in neurotransmitter levels. When a drug is repeatedly used, receptors in the brain become less sensitive to its effects, requiring higher doses to achieve the same result, as explained by the United States Drug Testing Laboratories Inc.
in “The Brain Chemistry Behind Tolerance and Withdrawal.” Simultaneously, neurotransmitter systems adjust—either by reducing production or altering receptor availability—to maintain balance in response to the drug’s presence. Over time, these adaptations diminish the drug’s impact, driving the cycle of tolerance.
This process is particularly evident with substances affecting dopamine and GABA pathways, such as opioids and sedatives.
What is the Key Mechanism for Drug Tolerance?
The key mechanisms for drug tolerance are metabolic tolerance and cellular tolerance. Metabolic tolerance occurs when the body becomes more efficient at metabolizing and eliminating a drug by increasing the activity of enzymes that break down the substance, as studied by the Canadian Society of Pharmacology and Therapeutics in “Metabolic drug tolerance ” This means that over time, the same dose of a drug is less effective because it is cleared from the system more quickly.
On the other hand, cellular tolerance refers to changes in the brain or body cells that reduce the drug’s effect at the receptor level, as studied by Grossman Z. et al. 1993, in “Cellular tolerance as a dynamic state of the adaptable lymphocyte.” This involves the downregulation of receptors or altered neurotransmitter levels, which reduce the drug’s ability to produce its intended effect. Both mechanisms contribute to the gradual need for higher doses to achieve the same response.
Contact us today to schedule an initial assessment or to learn more about our services. Whether you are seeking intensive outpatient care or simply need guidance on your mental health journey, we are here to help.
How Long Does It Take to Develop Drug Tolerance?
It takes several days to weeks for drug tolerance to develop, depending on factors like the type of drug and frequency of use, according to Healthline in “Understanding Drug Tolerance.” For example, tolerance to opioids develops after just two to three doses, as studied by Learn Genetics in “Opioids and the Physiology of Tolerance.” In contrast, tolerance to stimulants like cocaine takes several weeks.
Other factors, such as genetics, dose size, and metabolism, also influence the speed at which tolerance develops. Chronic exposure to a substance accelerates these changes in the brain and body, leading to a reduced response to the same drug dose over time.
What are Different Types of Drug Tolerance?
The different types of drug tolerance are pharmacodynamic tolerance, metabolic tolerance, and behavioral tolerance. Each type involves a unique process by which the body adapts to the presence of a drug over time.
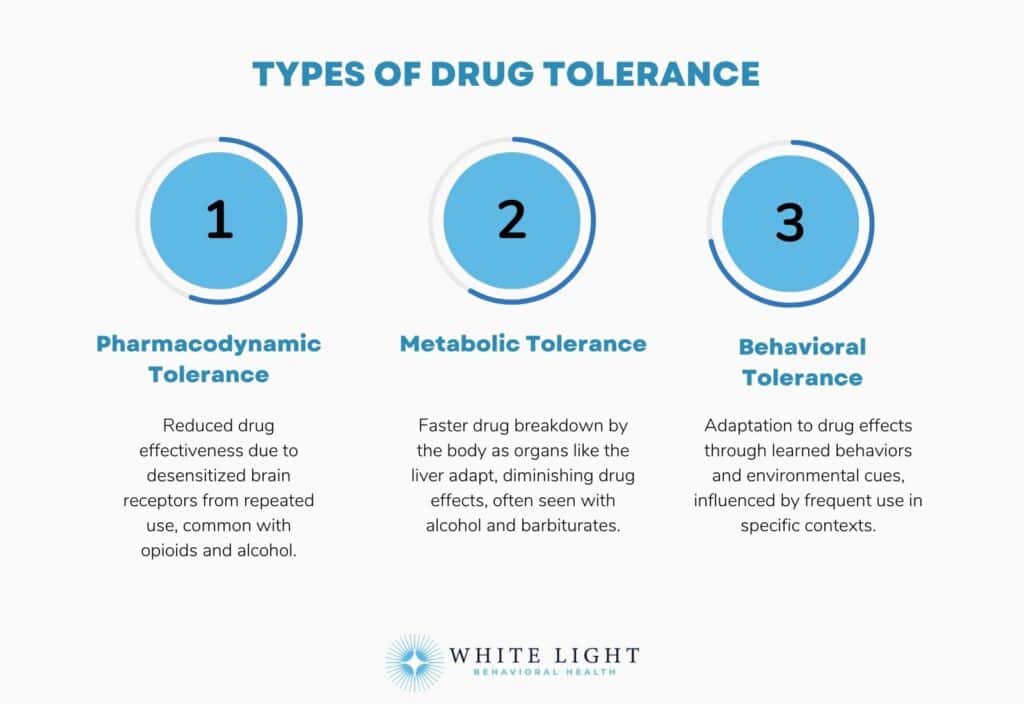
Following are the different types of drug tolerance:
- Pharmacodynamic Tolerance: Pharmacodynamic tolerance occurs when the drug’s effect is reduced due to changes in receptor sensitivity. With repeated exposure, the brain’s receptors become less responsive, meaning a person needs higher doses to achieve the same effect.
This form of tolerance is particularly significant in drugs that act directly on the central nervous system, such as opioids and alcohol, as studied by Stevens Negus, S et al. 2010, in “Pharmacodynamic Tolerance.”
- Metabolic Tolerance: Metabolic tolerance refers to the body’s ability to metabolize the drug more efficiently over time. As the liver or other organs adapt to process the drug more quickly, the drug’s effects diminish.
This type of tolerance occurs with substances like alcohol or barbiturates, where the body increases enzyme production to speed up the drug’s breakdown, as explained by Israel Y et al. 1979, titled “Studies on metabolic tolerance to alcohol, hepatomegaly, and alcoholic liver disease.”
- Behavioral Tolerance: Behavioral tolerance develops when individuals adapt their behavior due to the environment or habitual use of the drug. In situations where the individual is frequently exposed to the drug (like regular use in specific settings), the body becomes conditioned to the drug’s effects, leading to a tolerance that is influenced by learned behaviors rather than just physiological changes.
According to a study by Comley RE, Dry MJ, et al. 2020, titled “Acute Behavioral Tolerance to Alcohol,” the effect of alcohol on behavior decreases rapidly within a single dose, with subjective behavioral measures showing more consistent evidence of acute tolerance compared to objective performance-based tasks.
What Drugs and Substances Are Commonly Associated with Tolerance?
The drugs and substances that are commonly associated with tolerance include opioids, benzodiazepines, alcohol, stimulants, and nicotine. These substances require increasing doses over time to achieve the same effects due to the body’s physiological adaptations.
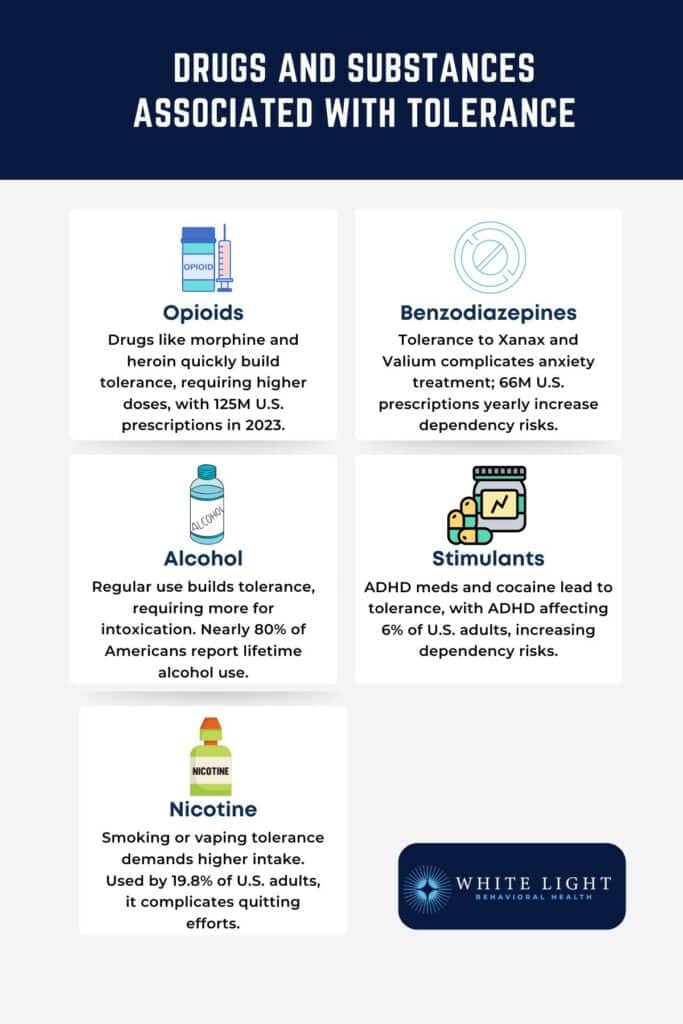
The following drugs and substances are commonly associated with tolerance:
- Opioids: Drugs like morphine, oxycodone, and heroin are highly associated with tolerance. With repeated use, the body’s receptors become less responsive, leading to a need for higher doses to manage pain or achieve euphoria.
This tolerance poses significant challenges in addiction treatment and pain management. Opioids are frequently prescribed, with approximately 125 million opioid prescriptions dispensed to American patients in 2023—with wide variation across states, as stated by the Centers for Disease Control and Prevention (CDC).
- Benzodiazepines: Medications such as diazepam (Valium) and alprazolam (Xanax) are used to treat anxiety and insomnia.
Prolonged use leads to tolerance, especially regarding sedative effects, making long-term management more complex in clinical settings. According to the Centers for Disease Control and Prevention (CDC), benzodiazepines are prescribed approximately 66 million times annually during office-based doctor visits in the United States, equating to about 27 prescriptions per 100 adults.
This high prescribing frequency significantly amplifies the issue of drug tolerance, as prolonged use increases the likelihood of patients requiring higher doses to achieve the same therapeutic effects, further complicating treatment and increasing dependency risks.
- Alcohol: Regular alcohol consumption results in tolerance, requiring higher quantities to achieve the same level of intoxication. Behavioral tolerance, where individuals adapt to functioning under the influence, is also a remarkable phenomenon.
Alcohol is widely accessible and commonly consumed, with 224.3 million people aged 12 and older (79.1% of this demographic) in the United States reporting lifetime alcohol use, according to the National Institute on Alcohol Abuse and Alcoholism (NIAAA) report, “Alcohol Use in the United States.” This prevalence underscores the substance’s social acceptance and potential for misuse.
- Stimulants: Drugs like amphetamines (used for ADHD) and cocaine lead to tolerance. Over time, their effects on alertness, energy, and euphoria diminish, increasing the risk of abuse and dependency.
The widespread use of stimulant medications for ADHD treatment has contributed to the growing issue of drug tolerance. With ADHD affecting a significant portion of the population—6% of adults and 10.5% of children in the U.S., as per the National Institute of Mental Health (NIMH)—the high prescription rates of stimulant medications like methylphenidate and amphetamines have made tolerance a more common concern.
As these medications are taken regularly, the body adapts, requiring higher doses to achieve the same therapeutic effects.
- Nicotine: Frequent use of nicotine, commonly through cigarettes or vaping, builds tolerance, requiring more frequent or higher doses to satisfy cravings. Nicotine tolerance contributes significantly to the difficulty of quitting smoking.
Nicotine use, prevalent in 19.8% of U.S. adults in 2022 (about 49.2 million people), contributes considerably to nicotine tolerance issues. As nicotine is regularly consumed, the body gradually adapts, requiring users to increase their intake to achieve the same effects, a key feature of nicotine tolerance.
This is particularly concerning given that tobacco use is most common among those aged 45-64 and more prevalent in men, according to the CDC.
How Does Drug Tolerance Affect the Body and Mind?
Drug tolerance affects the body and mind by diminishing the substance’s effectiveness over time, leading to the need for higher doses to achieve the same effects. Physiologically, this results in receptor desensitization, where cells respond less to the substance, and metabolic changes, as the body becomes more efficient at breaking down the drug, as studied by Schöneberg, T. et al. 2008, in “Tolerance and Desensitization.”
Psychologically, drug tolerance increases cravings as users seek to replicate the initial effects of the substance. Over time, this cycle heightens the risk of dependency, withdrawal symptoms, and potential overdose, further complicating recovery efforts.
What Risks are Associated with High Drug Tolerance Levels?
The risks associated with high drug tolerance levels include increased risk of overdose, physical health deterioration, and heightened dependency and addiction. As tolerance builds, individuals require larger doses to achieve the desired effect, which significantly increases the risk of accidental overdose, particularly with substances like opioids and benzodiazepines. Health deterioration arises as the body is subjected to greater strain, leading to organ damage, particularly in the liver and kidneys, and disruptions in necessary systems like the cardiovascular or respiratory systems.
The risks associated with high drug tolerance levels are as follows:
- Increased Risk of Overdose: High tolerance pushes individuals to consume larger doses, which surpass the body’s ability to process the drug safely. For instance, opioid overdose causes fatal respiratory depression because the central nervous system struggles to regulate breathing as the dosage increases beyond safe thresholds.
High-tolerance individuals are among the most vulnerable to fatal overdose during periods of relapse or changes in usage patterns. In 2022, the CDC reported 107,941 drug overdose deaths in the U.S., with an age-adjusted rate of 32.6 per 100,000 population.
- Physical Health Deterioration: Chronic high-dose consumption to overcome tolerance harms vital organs.
For example, long-term alcohol use causes liver cirrhosis, while chronic stimulant use leads to cardiovascular issues. As tolerance increases, the cumulative stress on these systems results in irreversible damage, complicating recovery efforts, as studied by Medical News Today in “What are the effects of drug misuse?”
- Heightened Dependency and Addiction: Tolerance fosters a deeper psychological dependency as users feel compelled to escalate use to maintain the desired effects.
This heightened dependency worsens behavioral health, contributes to compulsive substance use, and exacerbates mental health issues such as anxiety and depression. High tolerance is linked to more severe cases of addiction that are harder to treat due to the compounded physical and psychological challenges.
Rediscover Life at White Light Behavioral Health
Get the compassionate support you deserve.
We're here to help you reclaim joy, wellness, and a brighter future.
Our Facility
Who is Most Affected by Drug Tolerance?
Drug tolerance significantly affects individuals who engage in chronic substance use, particularly those dependent on opioids, benzodiazepines, or alcohol. High-risk groups also include individuals with mental health disorders, such as anxiety or depression, who use substances as self-medication and people in environments with consistent exposure to addictive substances. These groups require specialized treatment plans that address both the physiological changes of tolerance and underlying psychological conditions to prevent escalation to dependence or addiction.
Drug tolerance also affects individuals prescribed medications for legitimate medical purposes, such as managing chronic pain, anxiety, or seizure disorders. Over time, these patients require higher doses to achieve the same therapeutic effects, increasing the risk of side effects and potential dependence. For such cases, medical supervision is necessary to adjust treatment strategies, including drug rotation or combining non-pharmacological therapies, to mitigate the risks associated with tolerance development.
How is Drug Tolerance Assessed?
Drug tolerance is assessed by evaluating behavioral, physiological, and diagnostic indicators. This process involves self-reported symptoms, clinical observations, and specialized tools to determine the body’s reduced responsiveness to a substance. Understanding tolerance levels is important for guiding addiction treatment and ensuring safe medical interventions.
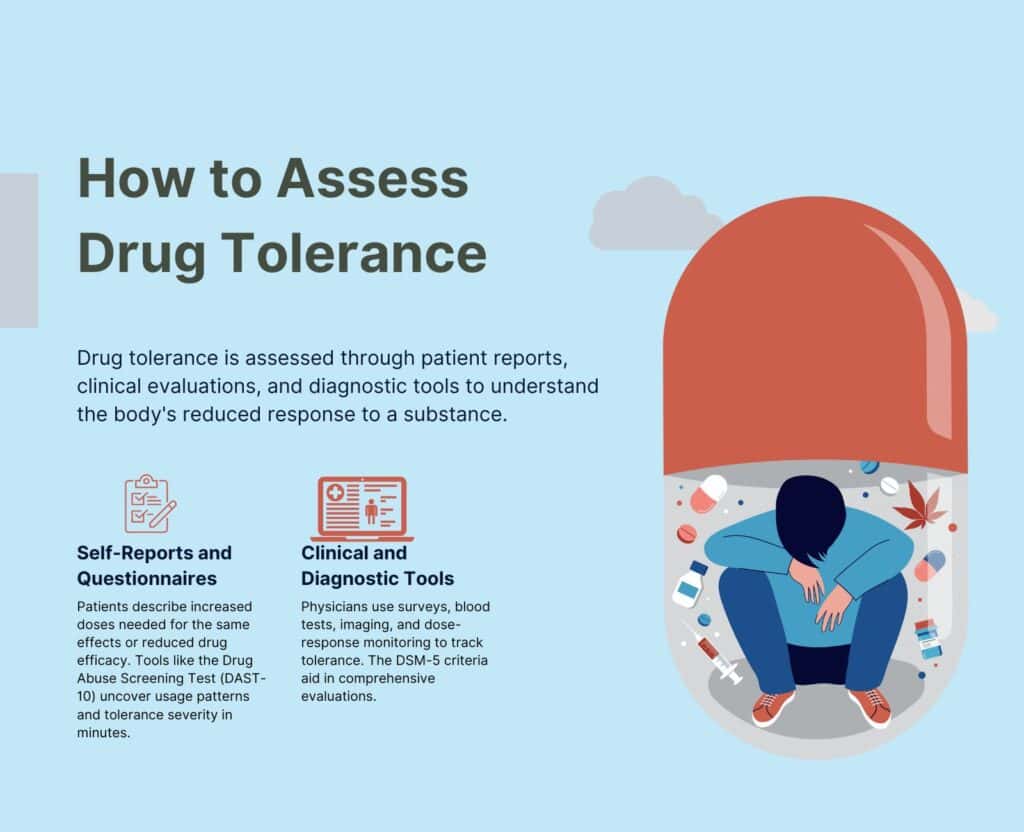
The following methods assess the drug tolerance:
- Key indicators and self-assessment questions: Patients report needing higher doses to achieve the same effect, experiencing reduced medication efficacy, or facing withdrawal symptoms between uses. Self-assessment questions help uncover patterns of escalating use and associated challenges.
Clinicians use this information to gauge the onset and severity of tolerance. For example, The Drug Abuse Screening Test (DAST-10) is an evidence-based tool widely used to assess the severity of psychoactive drug use.
It asks a series of yes or no questions about drug use over the past 12 months. It is either administered by a clinician or self-administered and completed in about 5 to 10 minutes.
- Diagnostic tools and processes used in addiction treatment: Tools such as standardized surveys, blood tests, or imaging scans measure the presence of substances and their impact on neural pathways.
In treatment settings, physicians might track dose-response relationships over time to monitor the development of tolerance and adjust medications or therapy accordingly. Research-backed tools like the DSM-5 criteria are integrated into clinical evaluations.
Why is Assessing Drug Tolerance Important?
Assessing drug tolerance is important to manage substance use disorders and tailor appropriate treatment plans effectively.
As tolerance develops, individuals require increasingly higher doses to achieve the same effect, leading to greater risks of overdose and physical harm. Proper assessment helps healthcare providers monitor these changes, adjust treatment protocols, and reduce the likelihood of dangerous side effects.
Accurately gauging tolerance levels prevents overdose, as higher tolerance masks the need for timely dose adjustments. Also, understanding an individual’s tolerance ensures that healthcare professionals provide safer and more effective treatment options, particularly when addressing withdrawal symptoms or managing medication dosages.
Monitoring tolerance is important for promoting recovery and preventing relapse, ultimately supporting safer, more individualized care strategies for those in rehabilitation or recovery from addiction.
What are the Short-term and Long-term Consequences of Drug Tolerance?
The short-term and long-term consequences of drug tolerance include the need for higher doses, the increased risk of physical dependency, and the potential for overdose.
The following are the short-term and long-term consequences of drug tolerance:
- Higher doses needed: As tolerance develops, individuals require progressively higher doses to achieve the same effects, which result in immediate risks such as drug misuse or overdose. This escalation in dosage increases the likelihood of harmful side effects, including respiratory depression and cardiovascular issues.
- Increased risk of dependency: Over time, the body becomes physically dependent on the substance, meaning individuals experience withdrawal symptoms when they reduce or stop usage.
This dependency results in the development of substance use disorders, making recovery more challenging. The psychological cravings and physical withdrawal lead to repeated substance use, further reinforcing addiction pathways in the brain.
- Overdose risk: With tolerance, the body’s reaction to a substance changes, and individuals are less aware of the severity of their intake, leading to the potential for overdose.
In extreme cases, a person ingests a fatal dose without realizing the consequences due to their increased tolerance levels. According to the National Center for Drug Abuse Statistics (NCDAS), drug overdose deaths have increased by 30% year-over-year, with over 96,700 fatalities annually, opioids contributing to 72% of these deaths, and nearly 1 million lives lost since 1999.
What is the Difference Between Drug Tolerance and Drug Dependence?
The main difference between drug tolerance and drug dependence lies in their nature and severity.
Tolerance refers to the body’s adaptation to a substance, requiring increasingly higher doses to achieve the same effect. However, this process does not necessarily involve withdrawal symptoms when the drug is reduced or discontinued.
In contrast, dependence represents a more advanced stage of addiction, where the body becomes physically reliant on the substance. With dependence, individuals experience withdrawal symptoms—such as anxiety, sweating, and shaking—when they try to stop or reduce use. Thus, while tolerance is about diminished effects over time, dependence includes a broader set of physiological changes and a psychological compulsion to continue using the substance to avoid these withdrawal effects.
Are you covered for treatment?
White Light Behavioral Health is an approved provider for Blue Cross Blue Shield and TUFTS, while also accepting many other major insurance carriers.
Check Coverage Now!How Can Drug Tolerance Lead to Addiction?
Drug tolerance can lead to addiction by causing individuals to gradually need higher doses of a substance to achieve the same effects. This escalation in tolerance drives people to continue using the drug in increasing amounts, increasing the risk of developing psychological dependency, physical dependence, and eventually addiction.
For substances like opioids and sedatives, where the effects on the central nervous system are profound, tolerance is particularly dangerous. As tolerance builds, users experience intense cravings and withdrawal symptoms when the drug is not used, reinforcing the cycle of addiction.
The connection between tolerance, withdrawal, and addiction is a central factor in how dependence develops over time. About 48.5 million (16.7%) Americans (aged 12 and older) battled a substance use disorder in 2023, according to a report by the Substance Abuse and Mental Health Services Administration (SAMHSA) titled “National survey on drug use and health.”
How Long Do Drug Tolerances Last?
Drug tolerance lasts for varying lengths of time, depending on the substance and individual factors. For many substances, tolerance persists as long as the drug is used continuously, with the body adjusting to the drug’s presence. However, tolerance begins to reverse once a person stops using the substance, within a few days to weeks, depending on the drug involved.
For example, with opioids, tolerance decreases within a few weeks of cessation, but it takes longer for other substances, like alcohol or benzodiazepines, where the body retains a certain level of tolerance for months. A study by Savic I, Widén L, Stone-Elander S. et al. 1997, titled “Feasibility of reversing benzodiazepine tolerance with flumazenil,” found that flumazenil, a benzodiazepine antagonist, was able to reverse tolerance to clonazepam in patients with partial seizures, offering seizure-free periods of 6 to 21 days without triggering withdrawal seizures, suggesting potential for intermittent therapy to manage benzodiazepine tolerance.
The duration of tolerance is influenced by factors such as the frequency of use, the dosage, and individual metabolic rates, with chronic users potentially experiencing longer-lasting tolerance. In some cases, if the substance is reintroduced, the tolerance returns more quickly due to “cross-tolerance” or the body’s previous adaptation to the substance.
What are Strategies to Manage and Reduce Drug Tolerance?
The strategies to manage and reduce drug tolerance include dose management, drug holidays and rotation, and behavioral interventions. These approaches help mitigate the need for increasing dosages, manage the risk of addiction, and improve overall treatment outcomes.
The strategies to manage and reduce drug tolerance are as follows:
- Dose Management: Dose management involves carefully adjusting the dosage of a drug over time to prevent excessive tolerance. By monitoring and lowering the dose gradually, patients avoid the escalating need for higher amounts of the substance.
Peper A. et al. 2009, titled “Aspects of the relationship between drug dose and drug effect,” show that this approach effectively minimizes the risks of developing tolerance while maintaining the drug’s therapeutic efficacy.
- Drug Holidays and Rotation: A drug holiday involves temporarily stopping the medication or rotating to a different drug to prevent the body from becoming overly tolerant. This is used with opioids and benzodiazepines.
Taking periodic breaks from opioids reduces long-term dependence and prevents tolerance from escalating. However, this strategy requires careful medical supervision to avoid withdrawal symptoms or relapse.
- Behavioral Interventions: Cognitive-behavioral therapy (CBT) and other psychological strategies are effective in managing cravings and reducing the psychological reliance on a substance.
These interventions help individuals develop coping mechanisms, address underlying psychological conditions, and reduce drug-seeking behavior. CBT is an important adjunct in addiction treatment, with significant evidence supporting its effectiveness in reducing substance use and improving long-term recovery outcomes.
What is the Role of Therapy in Managing Drug Tolerance?
The role of therapy in managing drug tolerance is important in addressing both the psychological and behavioral components of substance use.
Therapies such as Cognitive Behavioral Therapy (CBT), Dialectical Behavior Therapy (DBT), and Motivational Interviewing (MI) are important tools in helping individuals manage their tolerance to drugs and prevent further escalation of their substance use.
CBT is one of the most widely used therapeutic approaches in addiction treatment. It focuses on identifying and changing negative thought patterns and behaviors that contribute to substance use.
This approach helps individuals develop healthier coping mechanisms and reduce reliance on substances, which prevents the need for escalating drug doses due to tolerance. Approximately 60% of people who are treated with cognitive behavioral therapy for a substance use problem are able to maintain their recovery for a year, according to Verywell Mind.
Dialectical Behavior Therapy (DBT), an extension of CBT, is particularly effective for individuals with intense emotional responses. DBT teaches individuals to manage their emotions and develop coping strategies, reducing the likelihood of using substances as a means of emotional regulation.
A study by Dimeff LA and Linehan MM et al. 2008, titled “Dialectical behavior therapy for substance abusers,” found that individuals receiving Dialectical Behavior Therapy (DBT) were significantly more likely to remain in treatment, reduce substance abuse, and engage in individual therapy compared to those receiving standard treatments. Particularly, 64% of DBT participants stayed in treatment versus 27% in the control group, demonstrating DBT’s effectiveness for substance abuse management.
Motivational Interviewing (MI) is another important therapeutic tool in the treatment of drug tolerance. MI works by enhancing a person’s motivation to change by resolving ambivalence toward quitting or reducing substance use. MI helps individuals recognize the discrepancy between their current behavior and their values, which encourages them to take action toward reducing their drug use.
Motivational Interviewing (MI) is highly effective for addiction treatment, benefiting 75% of participants and being comparable to evidence-based methods like CBT. A study published in the Journal of Clinical Psychology found MI is up to 20% more effective than other treatments for alcohol use disorder. It also boosts client engagement by 15% and improves treatment retention when applied during intake.
Together, these therapeutic approaches provide a comprehensive strategy for managing drug tolerance by addressing both the psychological and emotional factors involved in substance use, which is important for long-term recovery and preventing further escalation of dependence.
What Medical Treatments Are Used to Address Drug Tolerance and Dependence?
The medical treatments that are used to address drug tolerance and dependence include a variety of medications and therapeutic interventions aimed at managing withdrawal symptoms, reducing cravings, and preventing relapse. These treatments play an integral role in helping individuals break free from the cycle of tolerance, escalation, and dependence.
The following medical treatments are commonly used:
- Opioid Agonists: Medications such as methadone or buprenorphine are used in opioid rehabilitation settings. These drugs help manage opioid dependence by binding to the same receptors in the brain, preventing withdrawal symptoms and cravings without producing the same high as opioids like heroin.
A study by Mattick RP, Breen C, Kimber J, and Davoli M. et al. 2009, titled “Methadone maintenance therapy versus no opioid replacement therapy for opioid dependence,” found that patients on methadone had 33% fewer opioid-positive drug tests and were 4.44 times more likely to remain in treatment compared to those not receiving opioid replacement therapy.
- Opioid Antagonists: Naloxone and naltrexone are opioid antagonists used to block the effects of opioids and prevent relapse. Naltrexone, for example, is used in both opioid and alcohol dependence treatment to reduce cravings and the reinforcing effects of substance use.
Its use in addiction treatment has been supported by research showing significant reductions in relapse rates.
- Benzodiazepine Tapering: In cases of benzodiazepine dependence, gradual tapering is employed to reduce tolerance and withdrawal risks. This approach involves slowly lowering the dosage over time to help the body adjust to lower levels of the substance, minimizing withdrawal symptoms and the potential for rebound anxiety.
- Alcohol Dependence Medications: Disulfiram, acamprosate, and topiramate are commonly used to treat alcohol dependence.
These medications work by either deterring drinking (disulfiram), reducing cravings (acamprosate), or modulating neurotransmitter activity to reduce the pleasurable effects of alcohol (topiramate).
- Antidepressants and Antipsychotics: In cases where drug dependence is associated with co-occurring mental health disorders, antidepressants or antipsychotics are prescribed to address underlying conditions like depression, anxiety, or mood disorders. These medications help manage symptoms that exacerbate cravings or contribute to substance abuse.
Did you know most health insurance plans cover substance use disorder treatment?
Can Drug Tolerance Be Reversed?
Yes, drug tolerance can be reversed in certain scenarios. The process depends on the type of drug and individual patient factors such as their health status, usage patterns, and the presence of any underlying conditions.
For some substances, such as opioids or alcohol, tolerance decreases with a period of abstinence, where the body regains sensitivity to the drug over time. However, this reversal varies.
For example, in opioids, the process of tolerance reduction is supported by medication-assisted treatments like methadone or buprenorphine, which help manage withdrawal while facilitating the reduction in tolerance levels. For other drugs, such as benzodiazepines, gradual tapering is used to reduce tolerance, minimizing withdrawal symptoms and risks. While tolerance decreases, it is not always fully reversed, particularly with long-term or high-dose usage.
How Can Drug Tolerance Be Prevented?
Drug tolerance can be prevented by incorporating strategies such as regular medical monitoring, employing therapies like CBT, and avoiding continuous high-dose exposure. These methods help minimize the body’s physiological adaptation to substances, reducing the likelihood of developing tolerance.
Drug tolerance is prevented using the following methods:
Regular Assessments
Healthcare providers conduct periodic evaluations to monitor the body’s response to medication. Adjusting dosages or timing based on these assessments prevents excessive tolerance development. Tapering dosages instead of abrupt changes reduces the risk of overuse.
CBT
Integrating cognitive-behavioral therapy (CBT) into treatment plans helps reduce drug dependency by addressing psychological triggers and maladaptive behaviors. By focusing on cognitive-behavioral therapy (CBT), clinicians teach patients to identify and reframe negative thought patterns, replacing them with healthier responses to stress or cravings. CBT is combined with medication, strengthens self-regulation and equips individuals with practical tools to manage triggers, thereby reducing reliance on pharmacological interventions.
Drug Rotation or Holidays
Strategically switching medications or taking breaks from certain substances allows the body to reset its sensitivity. This technique is commonly used in pain management with opioids to prevent tolerance buildup.
Contact us today to schedule an initial assessment or to learn more about our services. Whether you are seeking intensive outpatient care or simply need guidance on your mental health journey, we are here to help.
What are Alternative Approaches to Avoid Drug Tolerance Development?
The alternative approaches to avoid drug tolerance development include lifestyle modifications, non-drug therapies, and personalized medication strategies. These methods aim to reduce reliance on medications and promote holistic health management, thereby mitigating the risk of tolerance.
The alternative approaches to avoid drug tolerance development are as follows:
- Lifestyle changes: Regular physical activity, balanced nutrition, and adequate sleep improve overall health and decrease the need for long-term medication. For instance, a study by Sluka KA, Frey-Law L, Hoeger Bement M., et al. 2018, titled “Exercise-induced pain and analgesia?
Underlying mechanisms and clinical translation,” found that exercise has been shown to enhance natural pain-relief mechanisms, reducing dependence on analgesics.
- Non-drug therapies: Methods like acupuncture, mindfulness meditation, and physical therapy provide relief for conditions such as chronic pain or anxiety without increasing tolerance risk. A study by Priddy SE et al. 2018, titled “Mindfulness Meditation in the Treatment of Substance Use Disorders and Preventing Future Relapse: Neurocognitive Mechanisms and Clinical Implications,” found that the two primary mindfulness practices are focused attention and open monitoring to treat dependence effectively.
Cognitive-behavioral therapy (CBT), in particular, is effective in managing symptoms and reducing reliance on pharmaceuticals.
- Personalized medication strategies: Adjusting dosages, switching drug classes, or employing drug holidays under medical supervision allows the body to reset its response, decreasing the likelihood of tolerance buildup. These approaches ensure the medication remains effective over time.
When to Seek Help for Drug Tolerance?
You should seek help for drug tolerance when your medication no longer produces the desired effects, requiring higher doses to achieve the same relief, or when physical or psychological dependence begins to develop. Seeking professional assistance early helps prevent escalation to addiction or overdose.
The following are the signs that you need to seek help for drug tolerance:
- Increasing dosage requirements: If you notice that you need progressively larger amounts of a drug to achieve the same effect, it is time to consult a healthcare provider.
- Worsening symptoms despite usage: When the drug stops effectively managing the condition it was prescribed for, such as pain or anxiety, this indicates tolerance and requires help.
- Signs of dependence or cravings: Experiencing withdrawal symptoms, intense cravings, or using the drug outside of prescribed guidelines is a strong signal for professional intervention.
What is the Difference Between Drug Tolerance, Sensitization, and Desensitization?
The difference between drug tolerance, sensitization, and desensitization is rooted in how the body’s response to a substance changes over time due to repeated exposure. These processes involve variations in “receptor activity” and “neural adaptation,” impacting addiction and recovery.
The difference between drug tolerance, sensitization, and desensitization is explained below:
| Aspect | Drug Tolerance | Sensitization | Desensitization |
| Definition | A reduced response to a substance after repeated exposure, requiring higher doses to achieve the same effect. | An increased response to a substance with repeated exposure amplifies drug effects. | A decrease in receptor response due to constant stimulation by a substance. |
| Mechanism | Involves neural adaptation that diminishes drug effects or accelerates drug metabolism. | Involves heightened neural adaptation or changes that amplify sensitivity to a substance. | Occurs due to the downregulation of receptors or reduced receptor activity over time. |
| Examples | Opioid tolerance requires increased dosages for pain relief. | Cocaine use leads to more intense cravings and behavioral responses. | Chronic nicotine use reduces the ability of nicotine to stimulate dopamine release. |
| Impact on Rehab | This makes treatment challenging due to the higher doses needed, increasing overdose risk. | Heighten withdrawal symptoms, making detox emotionally or physically severe. | Recovery is complicated as desensitized systems require extensive time to reset normal functionality. |
| Relevance to Addiction | A precursor to dependence, leading to compulsive drug-seeking behavior. | Drives binge patterns or uncontrolled usage due to increased drug reinforcement. | Makes cessation difficult as natural reward systems become less responsive. |
| Management Approach | Gradual dose reduction, medication rotation, or drug holidays to reset tolerance. | Behavioral therapies to address cravings and manage sensitivity triggers. | Focused detox, receptor resetting, and alternative therapies to stabilize the system. |
Share This Post
















