Sugar Addiction: Symptoms, Causes, Effects, and Treatment

Sugar addiction refers to the compulsive consumption of sugar despite adverse consequences. It has become a widespread issue affecting people globally, with a notable prevalence in the United States.
Children are particularly vulnerable due to the accessibility of sugar-laden foods and beverages, contributing to unhealthy consumption patterns. According to DiNicolantonio et al. (2018) in the narrative review “Sugar Addiction: Is It Real?” sugar influences brain chemistry in ways similar to drug abuse, resulting in significant behavioral and health challenges.
The main symptoms of sugar addiction include cravings, tolerance, withdrawal, and binge eating. These behaviors closely resemble those seen in substance addiction, with individuals consuming progressively larger amounts of sugar to achieve the same satisfaction.
Withdrawal symptoms such as fatigue and irritability frequently appear when sugar intake is reduced. As noted by DiNicolantonio et al. (2018), sugar intake triggers dependence on natural opioids released during consumption, perpetuating its cycle.
The main causes of sugar addiction lie in the overstimulation of dopamine pathways. Repeated sugar intake drives a strong reward response in the brain, creating a cycle of compulsive consumption. Environmental factors, such as the prevalence of processed foods, combined with individual predispositions, further reinforce this behavior.
The notable effects of sugar addiction extend beyond physical health issues, including weight gain and metabolic diseases, to emotional disturbances like mood swings. These effects mimic the behavioral and neurochemical impact of other addictive substances. For instance, patterns such as craving and cross-tolerance align with those seen in substance addiction.
Treatment options for sugar addiction include behavioral therapies, holistic care, and structured plans such as a sugar detox program. Behavioral interventions focus on addressing patterns of excessive consumption, while holistic methods emphasize overall well-being, including improved nutrition and stress reduction.
A sugar detox program, which involves gradual withdrawal, has shown success in reducing dependency. Combining these treatments increases effectiveness by addressing both the psychological and physical aspects of sugar dependency.
More Resources on Addiction:
Sugar’s addictive potency surpasses that of many substances, including cocaine, as demonstrated in compelling animal studies. According to Lenoir, M., Serre, F., Cantin, L., & Ahmed, S. H. (2007), in the study “Intense Sweetness Surpasses Cocaine Reward,” 94% of rats consistently chose saccharin-sweetened water over intravenous cocaine, even when the cocaine dose was increased.
This preference persisted even in rats with a history of cocaine use or dependency, underscoring the intense reward sugar provides. The study further found that sugar activates dopamine signaling in the brain’s ventral striatum more robustly than cocaine, creating a powerful and potentially overriding reward signal.
What Is Sugar Addiction?
Sugar addiction is the compulsive overconsumption of sugar, characterized by an inability to control sugar intake despite negative health consequences. This behavior disrupts physical and emotional well-being and creates a cycle of craving, excessive consumption, and withdrawal. According to Westwater et al. (2016) in the review “Sugar Addiction: The State of the Science,” excessive sugar intake is linked to behavioral and neurochemical patterns similar to those observed in substance-related disorders.
Sugar is addictive because it activates the brain’s reward pathways, particularly dopamine systems. Repeated stimulation of these pathways reinforces the desire for sugar, leading to dependency. As noted by Westwater et al. (2016), excessive sugar intake contributes to patterns of tolerance and withdrawal symptoms that mirror those caused by other addictive substances.
Sugar is so addictive due to its ability to influence brain chemistry and behavior. It creates strong feelings of pleasure and reward, driving repetitive consumption. The effects of sugar on the brain are comparable to those of other substances, highlighting its powerful impact in fostering dependency.
Did you know most health insurance plans cover substance use disorder treatment? Check your coverage online now.
Is Sugar Addiction Real?
Sugar addiction is real, as evidenced by scientific analyses of its behavioral and neurochemical effects. The ongoing debate among experts focuses on whether excessive sugar intake causes brain changes and behaviors consistent with the criteria for addiction. According to Avena et al. (2008) in the review “Evidence for Sugar Addiction: Behavioral and Neurochemical Effects of Intermittent, Excessive Sugar Intake,” sugar meets four key markers of addiction: bingeing, withdrawal, craving, and cross-sensitization.
Scientific analysis shows that sugar activates the brain’s reward pathways by releasing opioids and dopamine, reinforcing repeated consumption. In controlled animal trials, rats given intermittent access to sugar exhibited binge-like patterns and dopamine release in the nucleus accumbens, a brain area linked to addiction. As noted by Avena et al. (2008), neural changes observed include shifts in dopamine receptor activity and enkephalin mRNA expression, effects that align with those produced by substances of abuse.
Withdrawal behaviors further highlight sugar’s addictive properties. In experiments, rats exhibited withdrawal symptoms when given naloxone, an opioid receptor blocker, or during periods of food deprivation. These outcomes suggest sugar engages the opioid system, contributing to dependency.
Although much of this work involves animal models, the similarities between sugar and addictive substances suggest implications for human issues, such as eating disorders and obesity. The neurochemical and behavioral responses to sugar closely mirror those of addictive drugs, reinforcing its role in addiction.
What Causes Sugar Addiction?
Sugar addiction stems from genetic, environmental, and emotional factors that contribute to dependency on excessive sugar consumption. These influences lead to behavioral patterns and brain changes that reinforce the cycle of addiction. According to Jacques et al. (2019) in the review “The Impact of Sugar Consumption on Stress Driven, Emotional and Addictive Behaviors,” long-term sugar consumption alters neural pathways, impairing impulse control and increasing dependency.

1. Genetic and Biological Predisposition
Genetic susceptibility and brain responses play a significant role in sugar addiction.
Variations in genetics determine how individuals process sugar and their likelihood of developing dependency. Sugar consumption stimulates dopamine release, activating reward pathways in the brain and reinforcing the drive for more consumption.
Prolonged sugar intake disrupts dopamine receptor activity, leading to a neurochemical imbalance that diminishes self-regulation and sustains dependency.
2. Environmental and Cultural Triggers
Societal norms and the availability of sugar-rich foods intensify sugar addiction.
Food marketing promotes sugary products aggressively, embedding them into daily habits. Societal habits, such as associating sugar with celebrations and routines, normalize frequent consumption.
High sugar accessibility, especially in Western countries, has made overconsumption widespread. Jacques et al. (2019) highlighted that such factors contribute to rising obesity rates, with 67.9% of adults in the United States classified as overweight in 2016.
3. Emotional Stress and Comfort Eating
Emotional connections to sugar consumption drive dependency through emotional eating and stress-related behaviors.
Sugar provides stress relief by triggering neurochemical responses that temporarily improve mood. Many individuals turn to sugar as a comfort food during periods of emotional distress.
Long-term sugar consumption alters the dopaminergic system, causing neuronal changes and heightened emotional responses, which reinforce addiction.
Contact us today to schedule an initial assessment or to learn more about our services. Whether you are seeking intensive outpatient care or simply need guidance on your mental health journey, we are here to help.
What Is Your Body Lacking When Craving Sugar?
What your body is lacking when craving sugar includes key nutrients such as magnesium, chromium, or serotonin precursors, which contribute to a nutrient imbalance. These deficits disrupt energy regulation, mood balance, and appetite control, leading to increased sugar cravings. According to Freeman et al. (2018) in the review “Impact of Sugar on the Body, Brain, and Behavior,” sugar consumption influences the brain’s reward system, reinforcing cravings and behaviors associated with addiction.
Low levels of magnesium contribute to sugar cravings by affecting energy production and nerve function. Magnesium supports blood sugar regulation, and a deficiency disrupts glucose control, leading to fatigue and irritability that drive the desire for quick energy from sugar.
A lack of chromium interferes with the body’s ability to stabilize blood glucose levels. Chromium enhances insulin efficiency, reducing energy fluctuations that trigger cravings. Insufficient chromium leads to more frequent energy crashes and an increased urge for sugary foods to restore balance.
Serotonin deficiencies also play a role in sugar cravings. As a neurotransmitter that affects mood and appetite, low serotonin levels lead to feelings of sadness or stress, driving individuals to seek sugar for its temporary soothing effects. Serotonin depends on nutrients like tryptophan, and inadequate intake of these precursors heightens cravings.
Freeman et al. (2018) noted that excessive sugar intake disrupts nutrient absorption and neurochemical balance, perpetuating the cycle of cravings and reinforcing addictive behaviors. Correcting these nutrient imbalances through a diet rich in magnesium and chromium supports better energy regulation and reduces dependency on sugar.
What Roles Do Dopamine and Reward Pathways Play in Sugar Addiction?
Dopamine and reward pathways play a central role in sugar addiction by reinforcing behaviors linked to sugar consumption through the brain’s reward mechanism. When sugar is consumed, dopamine is released in neural pathways associated with pleasure and reward, creating a sense of satisfaction that drives repetitive behavior. According to Greenberg et al. (2021) in the review “Sugars and Sweet Taste: Addictive or Rewarding?” the neural responses triggered by sweet tastes activate circuits similar to those engaged by substances of abuse, highlighting the powerful reinforcement associated with sugar consumption.
The reward mechanism linked to sugar consumption depends on its palatability rather than its nutritional value. Sweet tastes stimulate brain regions, including the nucleus accumbens, which are associated with anticipation and pleasure.
This activation strengthens the connection between sugar intake and feelings of reward, encouraging overconsumption. This behavior reflects the reward value of sugar rather than a metabolic requirement for calories.
While sugar impacts dopamine systems in ways that resemble addictive substances, Greenberg et al. (2021) argued that the reward pathways associated with sugar consumption are distinct from those of addiction. The review concluded that focusing on the reward value of sugar provides a clearer understanding of overconsumption and its role in reinforcing unhealthy eating behaviors.
What Are the Symptoms and Signs of Sugar Addiction?
The symptoms and signs of sugar addiction include physical, emotional, and psychological indicators that reflect dependency on excessive sugar intake. These symptoms manifest through cravings, withdrawal, compulsive behavior, and disruptions in emotional regulation. According to Garber et al. (2011) in the review “Is Fast Food Addictive?” sugar consumption contributes to patterns of tolerance and withdrawal similar to addictive behaviors, emphasizing the impact of high sugar intake on physical and emotional health.
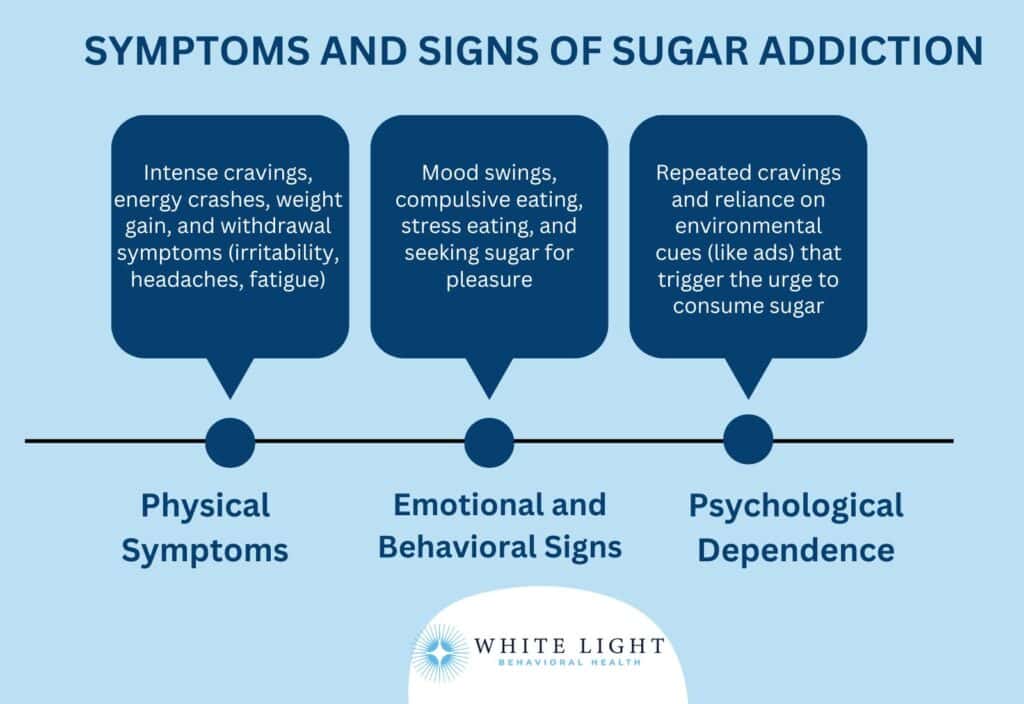
1. Physical Symptoms of Sugar Addiction
- Cravings: Intense urges for sugary foods, particularly in response to stress or fatigue.
These cravings lead to overconsumption of sugar-laden products.
- Energy spikes and crashes: A temporary energy boost after sugar intake is followed by lethargy or fatigue as blood sugar levels drop.
- Weight gain: Regular sugar consumption contributes to a caloric surplus and leads to obesity, with obese adults consuming more sugar-rich fast food compared to others, as noted by Garber et al. (2011).
- Withdrawal symptoms: Irritability, headaches, and fatigue when sugar intake is reduced, resembling withdrawal patterns seen in addictive substances.
2. Emotional and Behavioral Indicators
- Mood swings: Mood swings include frequent highs and lows in mood due to the fluctuating blood sugar levels caused by excessive sugar intake.
- Compulsive eating: Compulsive eating refers to an inability to resist sugary foods, even when not hungry, reflecting patterns of compulsive behavior.
- Stress eating: Stress eating involves relying on sugary foods as a coping mechanism during emotional stress, reinforcing unhealthy eating habits.
- Reward-seeking behavior: Reward-seeking behavior describes seeking sugary foods to stimulate pleasure or reward pathways in the brain.
Rediscover Life at White Light Behavioral Health
Get the compassionate support you deserve. We're here to help you reclaim joy, wellness, and a brighter future.

3. Psychological Dependence on Sugar
Psychological dependence on sugar is driven by repeated craving cycles and behaviors linked to the brain’s reward system.
Sugar consumption activates neural circuits associated with pleasure and reinforces compulsive behavior, making it difficult to break the dependency. Garber et al. (2011) emphasized that environmental cues, such as fast food advertisements and sugary product availability, exacerbate this dependency by triggering cravings.
These behaviors align with patterns seen in other addictive substances, further illustrating sugar’s role in reinforcing psychological dependency.
How Does Sugar Addiction Affect the Body?
Sugar addiction affects the body by disrupting metabolic processes, altering brain function, and contributing to long-term health issues. Excessive sugar intake leads to cycles of dependency, with effects on energy regulation, emotional stability, and physical well-being. According to Garber et al. (2011) in the review “Is Fast Food Addictive?”, sugar consumption reinforces patterns of craving and dependency, contributing to chronic diseases such as obesity, diabetes, and hypertension.
Excessive sugar intake is a major factor in weight gain, with the average American consuming 15 to 19 teaspoons daily, far exceeding recommended limits. High sugar consumption also increases the risk of type 2 diabetes and cardiovascular disease, with those consuming over 17% of their calories from sugar facing a 38% higher risk of heart-related death compared to lower sugar consumers.
Reducing added sugar intake is essential for mitigating these health risks.
Metabolic Impacts of Excess Sugar
The metabolic impacts of excess sugar include insulin resistance, a higher risk of obesity, and fluctuating blood sugar levels. Prolonged sugar consumption disrupts insulin activity, impairing the body’s ability to manage glucose effectively.
This dysfunction increases fat storage and promotes weight gain. Garber et al. (2011) noted that obese adults are more likely to consume sugar-rich fast foods, worsening these effects.
Frequent sugar intake also causes dramatic swings in blood sugar, creating cycles of energy spikes and crashes that reinforce dependency.
Impact on Brain Chemistry and Mental Health
Sugar addiction impacts brain chemistry by activating reward pathways that influence behavior and mood. Excess sugar stimulates dopamine release, reinforcing patterns of consumption linked to cravings.
Over time, this activity reduces dopamine receptor sensitivity, impairing the brain’s ability to regulate emotions and increasing vulnerability to conditions like ADHD, anxiety, and depression. According to Greenberg et al. (2021) in the review “Sugars and Sweet Taste: Addictive or Rewarding?” these neural changes contribute to compulsive behavior and emotional instability, worsening symptoms of these conditions, and perpetuating the dependency cycle.
Physical Health Consequences
- Weight gain: High sugar intake promotes excess calorie consumption and fat storage, contributing to obesity.
- Inflammation: Chronic sugar consumption increases inflammation and is linked to cardiovascular issues and joint pain.
- Dental problems: Sugary diets encourage tooth decay due to increased bacterial activity in the mouth.
- Energy crashes: Frequent sugar consumption causes short-term energy spikes followed by significant drops in physical stamina.
Are you covered for treatment?
White Light Behavioral Health is an approved provider for Blue Cross Blue Shield and TUFTS, while also accepting many other major insurance carriers.
Long-Term Impacts on Energy Levels
The long-term impacts of sugar addiction on energy levels include chronic fatigue and disruptions to the circadian rhythm. Excess sugar places strain on the adrenal glands, leading to adrenal fatigue that reduces the body’s ability to maintain consistent energy.
This cycle is further exacerbated by repeated energy crashes caused by unstable blood sugar levels. According to Freeman et al. (2018) in the review “Impact of Sugar on the Body, Brain, and Behavior,” the reliance on sugar undermines the body’s ability to regulate energy naturally, perpetuating exhaustion over time.
How Is Sugar Addiction Diagnosed?
Sugar addiction is diagnosed through tools and questionnaires designed to assess patterns of excessive sugar consumption and its impact on health and behavior. According to Witek et al. (2022) in the review “A High-Sugar Diet Consumption, Metabolism and Health Impacts with a Focus on the Development of Substance Use Disorder: A Narrative Review,” sugar addiction shares characteristics with substance use disorders.
The prevalence of food addiction is higher among women (24.9%) and individuals over 35 years old (22.2%). Tools like the YFAS and self-assessment questionnaires help identify individuals at risk, allowing them to seek appropriate interventions for sugar dependency.
- Yale Food Addiction Scale (YFAS): The YFAS evaluates food addiction by measuring behaviors such as loss of control, cravings, and inability to reduce consumption of foods like those high in sugar.
- Self-reported questionnaires: These assessments focus on dietary patterns, emotional responses to sugar consumption, and physical symptoms of withdrawal to identify potential addiction.
- Behavioral and health assessments: Clinicians assess behavioral patterns like binge eating and health metrics such as obesity or Type 2 diabetes prevalence, which affects approximately 11.3% of the U.S. population, or 37.3 million people, according to the CDC’s 2022 National Diabetes Statistics Report, to support a diagnosis of sugar addiction.
Self-assessment Questions for Sugar Addiction
- Do you experience intense cravings for sugary foods that interfere with your daily activities?
- Have you noticed a need to consume more sugar over time to feel satisfied?
- Do you feel irritable, anxious, or fatigued when you reduce or stop sugar consumption?
- Do you rely on sugary foods to manage stress or improve your mood?
- Have you attempted to cut back on sugar intake but found it challenging to maintain?
What Are the Early Warning Signs That You Are Addicted to Sugar?
The early warning signs that you are addicted to sugar include behavioral, physical, and emotional patterns related to sugar consumption. These signs reflect dependency and its impact on daily life. According to Garber et al. (2011) in the review “Is Fast Food Addictive?,” sugar consumption activates the brain’s reward system, creating patterns of compulsive behavior and dependency such as binge eating and mood swings..

The early warning signs of sugar addiction are defined below:
- Cravings: Intense, uncontrollable urges for sugary foods, especially during times of stress or fatigue.
- Binge eating: Consuming large amounts of sugar in one sitting, accompanied by feelings of guilt or lack of control.
- Energy crashes: Experiencing fatigue and lethargy after the temporary energy boost from sugar has worn off.
- Mood swings: Fluctuations in mood, including irritability or sadness, tied to changes in blood sugar levels.
- Failed attempts to cut back: Repeated efforts to reduce sugar intake that result in relapses or heightened cravings.
Can Children Be Addicted to Sugar?
Yes, children can exhibit addictive-like behaviors toward sugar due to its impact on their developing brains and its role in reinforcing dependency. Excessive consumption of sugar-sweetened beverages (SSBs) contributes significantly to this issue. According to Calcaterra et al. (2023) in the review “Sugar-Sweetened Beverages and Metabolic Risk in Children and Adolescents with Obesity,” SSBs are the primary source of free sugars in children’s diets, with a single 12-fluid-ounce soda containing 35.0–37.5 g of sugar and 140–150 calories.
Sugar marketing heavily targets children, normalizing frequent consumption of sugary drinks and snacks. This marketing strategy amplifies dependency, creating long-term patterns of overconsumption.
These behaviors directly contribute to childhood obesity, with children in the highest quartile of SSB intake having 3.20 times higher odds of developing metabolic syndrome than those in the lowest quartile. High SSB intake also increases the risk of abdominal obesity by 2.49 times and hypertension by 2.79 times, reinforcing the health risks associated with excessive sugar consumption.
Did you know most health insurance plans cover substance use disorder treatment? Check your coverage online now.
What Are Treatment Options for Sugar Addiction?
Treatment options for sugar addiction include detox strategies, therapies, medical interventions, and holistic lifestyle changes that address dependency and support recovery. According to Calcaterra et al. (2023) in the review “Sugar-Sweetened Beverages and Metabolic Risk in Children and Adolescents with Obesity,” these approaches are designed to manage cravings, improve overall health, and reduce the impact of sugar consumption on the brain’s reward system.
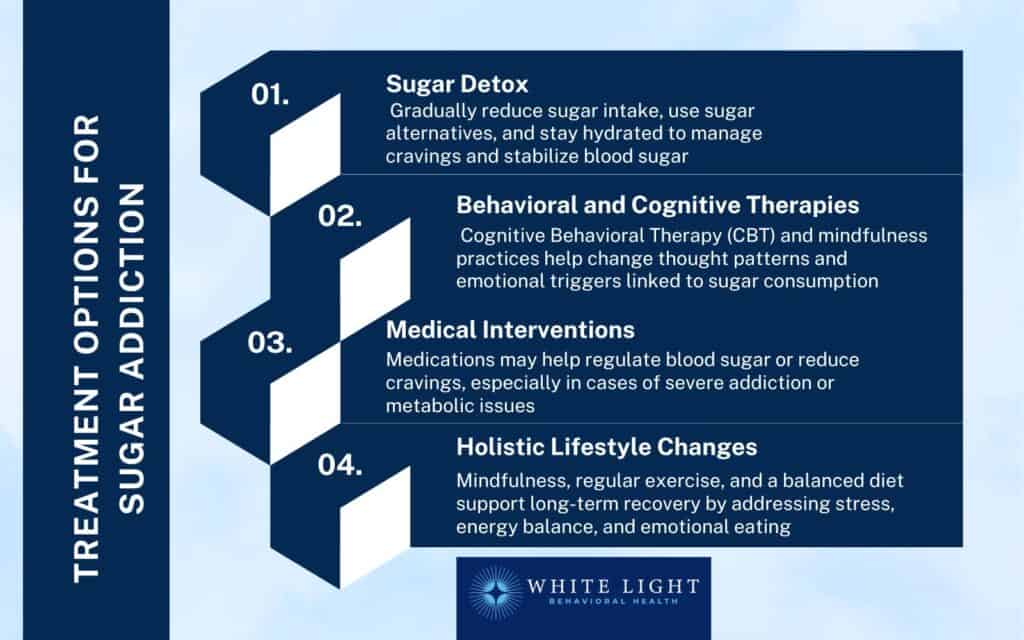
1. Sugar Detox Strategies
Sugar detox strategies involve gradually reducing sugar intake, incorporating sugar alternatives, and increasing hydration to minimize cravings.
Gradual reduction helps stabilize blood sugar levels and prevents withdrawal symptoms, which include headaches, fatigue, irritability, and intense cravings if sugar is quit cold turkey. Sugar alternatives like natural sweeteners provide satisfaction without triggering dependency.
Hydration is important as thirst mimics sugar cravings. Detox periods last one to three weeks, depending on the individual.
According to Calcaterra et al. (2023), sugar detox methods are effective in breaking cycles of overconsumption and stabilizing energy levels.
2. Behavioral and Cognitive Therapies
Behavioral and Cognitive Therapies help address the psychological drivers of sugar addiction by improving coping strategies and emotional regulation.
They are particularly effective for breaking patterns of dependency and fostering long-term behavior change. Among these, Cognitive Behavioral Therapy (CBT) is the most effective for sugar addiction, as it targets the thoughts and behaviors that sustain cravings and binge eating.
Below are key therapeutic approaches for managing sugar addiction:
- Cognitive Behavioral Therapy (CBT): CBT helps individuals identify and change negative thought patterns associated with sugar cravings and binge eating.
- Mindfulness-Based Stress Reduction (MBSR): MBSR teaches individuals to manage stress and emotional eating through mindfulness practices.
- Group Therapy: Support groups provide accountability and shared experiences, fostering motivation to overcome sugar addiction.
3. Medical and Pharmacological Interventions
Medical and pharmacological interventions include treatments such as medications to stabilize blood sugar levels or manage withdrawal symptoms.
For individuals with severe sugar dependency, physicians prescribe treatments aimed at reducing cravings or supporting metabolic health. According to Calcaterra et al. (2023), these interventions are effective when combined with dietary and behavioral strategies, especially in managing withdrawal symptoms and preventing relapse.
4. Holistic Lifestyle Adjustments
Holistic lifestyle adjustments focus on creating overall balance in the body and mind to reduce the reliance on sugar as a source of comfort or energy. By addressing underlying stress, nutritional imbalances, and sedentary habits, these strategies and mindfulness empower individuals to manage cravings naturally.
Below are key holistic approaches to support sugar addiction recovery:
- Mindfulness practices: Techniques such as meditation help regulate stress, reducing the emotional triggers that lead to sugar cravings.
- Regular exercise: Physical activity improves mood and balances blood sugar, decreasing dependency on sugar for energy or emotional relief.
- Balanced diet: A nutrient-rich diet reduces cravings by stabilizing blood sugar levels and ensuring the body gets essential nutrients.
Are Artificial Sweeteners a Good Alternative for Managing Sugar Addiction?
Yes, artificial sweeteners are a good alternative for managing sugar addiction due to their ability to reduce sugar intake, but they raise concerns about potential health impacts and dependency. These sugar substitutes provide sweetness without the calories or blood sugar spikes of regular sugar, which helps in reducing cravings and stabilizing energy levels. Artificial sweeteners reinforce craving cycles by continuing to stimulate the brain’s reward system without addressing underlying dependency. According to Calcaterra et al. (2023) in the review “Sugar-Sweetened Beverages and Metabolic Risk in Children and Adolescents with Obesity,” while artificial sweeteners help manage sugar consumption, their long-term efficacy and impact on addiction require further evaluation.
Contact us today to schedule an initial assessment or to learn more about our services. Whether you are seeking intensive outpatient care or simply need guidance on your mental health journey, we are here to help.
How Long Does It Take to Break a Sugar Addiction?
Breaking a sugar addiction takes several weeks to months, with cravings being strongest during the first six months of recovery. Eating every three to five hours helps stabilize blood sugar levels and manage cravings effectively. Consistent strategies such as meal planning and gradual reduction are key to reducing dependency. According to Witek et al. (2022) in the review “A High-Sugar Diet Consumption, Metabolism and Health Impacts with a Focus on the Development of Substance Use Disorder: A Narrative Review,” sugar cravings during recovery are linked to neuroadaptations, emphasizing the importance of routine and persistence in treatment.
When Should You Seek Professional Help for Sugar Addiction?
You should seek professional help for sugar addiction when cravings and dependency interfere with daily life or lead to physical, emotional, or behavioral health issues. Signs include an inability to control sugar intake, binge eating, withdrawal symptoms like irritability or fatigue, and using sugar to manage stress or emotions. A professional sugar detox program is also recommended if sugar consumption contributes to obesity, Type 2 diabetes, or other metabolic disorders.
Support is found through registered dietitians, addiction specialists, and therapists experienced in behavioral and cognitive therapies. According to Witek et al. (2022) in the review “A High-Sugar Diet Consumption, Metabolism and Health Impacts with a Focus on the Development of Substance Use Disorder: A Narrative Review,” sugar addiction shares similarities with substance use disorders, making targeted interventions important for recovery.
How Does Sugar Addiction Compare to Other Addictions?
Sugar addiction compares to other addictions by affecting the brain’s reward pathways and reinforcing compulsive behaviors through similar neurochemical processes. While it lacks the immediate physical dangers of substances like heroin or methamphetamine, sugar creates cycles of dependency and cravings that parallel other addictive substances over time.
The following comparisons examine sugar addiction alongside other common addictions, focusing on its neurochemical effects, behavioral patterns, and health consequences.
- Sugar vs. Cocaine: Sugar affects the brain’s dopamine pathways similarly to cocaine, triggering repeated consumption.
According to Witek et al. (2022), both substances create neuroadaptations that reinforce dependency and compulsive behaviors.
- Sugar vs. Nicotine: Sugar impacts mood and energy regulation, while nicotine creates more immediate and intense chemical dependence.
According to Avena, N. M., Rada, P., & Hoebel, B. G. (2008) in the review “Evidence for Sugar Addiction: Behavioral and Neurochemical Effects of Intermittent, Excessive Sugar Intake,” both substances stimulate dopamine release but through different mechanisms. While sugar consumption leads to dependence-like behaviors and changes in dopamine and opioid receptor binding, nicotine’s stronger physical and psychological dependence makes it more severe.
However, sugar’s ubiquity in 75% of packaged foods and its role in modern diets make its dependency a significant public health challenge.
- Sugar vs. Heroin: Heroin causes severe withdrawal symptoms and physical health risks, while sugar more subtly impacts the reward system, leading to long-term compulsive consumption patterns.
- Sugar vs.
Marijuana:
Sugar primarily affects energy levels and emotional regulation, while marijuana has psychoactive effects. According to Volkow, N. D., Koob, G. F., & McLellan, A. T. (2016) in the review “Neurobiologic Advances from the Brain Disease Model of Addiction,” both substances activate the brain’s reward system via dopamine release, but through different mechanisms.Marijuana’s THC acts on the endocannabinoid system, whereas sugar influences multiple neurotransmitters. While approximately 9% of marijuana users develop addiction, sugar’s behavioral dependency is more ingrained due to its accessibility and role in daily diets, making it a pervasive public health concern.
- Sugar vs.
Caffeine:
Sugar vs. Caffeine: Sugar primarily contributes to metabolic disorders, while caffeine affects energy and alertness.According to Zwyghuizen-Doorenbos, A., Roehrs, T. A., Lipschutz, L., Timms, V., & Roth, T. (1990) in the study “Effects of Caffeine on Alertness,” sugar consumption is linked to metabolic issues like obesity and diabetes due to blood glucose imbalances, whereas caffeine enhances alertness and reduces fatigue by stimulating the central nervous system. Both substances can lead to dependency, with caffeine withdrawal causing headaches and irritability, and excessive sugar intake increasing the risk of chronic diseases such as heart disease.
- Sugar vs.
Alcohol:
Sugar and alcohol both influence mood and are linked to binge consumption. Alcohol poses immediate risks to mental and physical health, while sugar’s effects develop over time. - Sugar vs.
Cigarettes:
Cigarettes directly harm the lungs and heart, while sugar contributes to systemic issues like obesity and diabetes. Both substances activate dopamine pathways that drive dependency. - Sugar vs.
Methamphetamine:
Methamphetamine has extreme neurochemical effects, but sugar similarly reinforces cravings through its impact on dopamine release. Sugar dependency is driven by long-term exposure rather than acute intoxication. - Sugar vs.
Opium:
Sugar does not produce narcotic effects like opium, but both engage the brain’s reward system over time, encouraging repetitive use and compulsive behaviors.
Share This Post
















