Fentanyl: Definition, Uses, Side Effects, and Overdose Risks

Fentanyl, a highly potent medication, is prescribed to relieve intense pain, particularly for patients recovering from surgery or undergoing cancer treatment. Classified as a Schedule II drug under the Controlled Substances Act, fentanyl is available in various forms, including patches, lozenges, and injections, with carefully monitored dosages to prevent misuse.
According to the results from the 2021 National Survey on Drug Use and Health, around 539,000 people aged 12 or older misused prescription fentanyl, making up nearly 21% of all users. That year, fentanyl-related cases led to 122,884 ER visits, with the highest rates among individuals aged 26-44.
The uses of fentanyl include managing severe pain in cancer patients, post-surgical recovery, and individuals with chronic pain who are tolerant to other opioids. It is available in patches, lozenges, injections, and nasal sprays for precise pain relief.
In medical settings, fentanyl is also used as an anesthetic adjunct during surgeries. Due to its rapid onset and effectiveness, it is important for pain management in controlled environments but carries a high risk of misuse and overdose if not used as prescribed.
Common side effects of fentanyl include drowsiness, nausea, confusion, dizziness, and respiratory depression. Prolonged use leads to fentanyl addiction, as the drug alters brain chemistry, reinforcing compulsive drug-seeking behavior. Individuals using fentanyl for extended periods also develop tolerance and physical dependence, requiring higher doses for the same effects.
The risk of fentanyl overdose is extremely high, especially without medical supervision, with symptoms including slowed breathing, loss of consciousness, pinpoint pupils, and cold, clammy skin. Respiratory failure is the primary cause of death, as studied by Zhuang J et al. 2024 in “Cardiorespiratory failure induced by inhalation of aerosolized fentanyl in anesthetized rats.” Illicit fentanyl has fueled the U.S. opioid crisis, mixed with heroin, cocaine, and counterfeit pills, increasing overdose deaths.
With potency 50 to 100 times stronger than morphine, even small amounts are fatal. The CDC reports that fentanyl was involved in approximately 70,000 U.S. overdose deaths in 2021, making it a leading cause of opioid-related fatalities.
What Is Fentanyl?
Fentanyl is a synthetic opioid analgesic that is significantly more potent than morphine. Fentanyl is approximately 50 to 100 times stronger than morphine, as reported by NIH. A new report released by the Centers for Disease Control and Prevention (CDC) found an estimated 70% of overdose deaths involved fentanyl, with over 93,000 opioid-related deaths reported between June 2023 and June 2024.
More Resources on Addiction:
It is primarily used in medical settings as a prescription medication to manage severe pain, especially in cancer patients or those undergoing surgery. However, illegal fentanyl is also illicitly manufactured and distributed, mixed with other drugs, increasing the risk of overdose. Due to its extreme potency, even small amounts are deadly, making it a major contributor to the ongoing opioid crisis.
Did you know most health insurance plans cover substance use disorder treatment? Check your coverage online now.
What Are the Different Forms of Fentanyl?
Different forms of fentanyl are prescription patches, lozenges, injections, and illicit forms like powder, pressed pills, and fentanyl-laced drugs. Prescription fentanyl is carefully dosed and used for managing severe pain, with patches providing slow-release, lozenges offering quick relief, and injections used in medical procedures and emergencies. On the other hand, illicit fentanyl, found in powder or counterfeit pill form, is highly potent and unpredictable, increasing the risk of overdose, especially when mixed unknowingly into fentanyl-laced drugs like heroin or cocaine.

Different forms of fentanyl are as follows:
- Transdermal Patches: These are prescribed to manage chronic pain by slowly releasing fentanyl through the skin over time. They provide long-lasting pain relief and are used for patients with severe, persistent pain.
- Lozenges (Lollipops): Lozenges, also known as oral transmucosal fentanyl, are fast-acting prescription medications designed for breakthrough pain.
This form of fentanyl is used by cancer patients.
- Injections: Injectable fentanyl is administered in medical settings and used for anesthesia, post-surgical pain management, and emergencies that require strong pain relief.
- Powder: Illicit fentanyl is commonly found in powder form, which is extremely potent and mixed with other drugs, making it highly dangerous and unpredictable.
- Pressed Pills: Pressed pills are counterfeit pills that are made to resemble prescription opioids like oxycodone or benzodiazepines but contain fentanyl, increasing the risk of overdose.
- Fentanyl-Laced Drugs: Illicit fentanyl is frequently mixed with heroin, cocaine, and other substances without the user’s knowledge, leading to a high risk of fatal overdoses.
What Are the Street Names of Fentanyl?
The street names of fentanyl are China White, Tango & Cash, Apache, Dance Fever, Goodfella, and Jackpot. These names reflect the potency, effects, or origins in the illicit drug trade.
For example, “China White” refers to its appearance as a white powder, while “Apache” is linked to its strength, comparable to a powerful warrior. Dealers and users use these code names to disguise transactions and evade law enforcement.
The street names of fentanyl are as follows:
- China White
- Tango & Cash
- Apache
- Dance Fever
- Goodfella
- Jackpot
How Is Fentanyl Used Medically?
Fentanyl is medically used to treat severe pain in patients undergoing surgery, those with cancer, and individuals needing palliative care. It is an FDA-approved opioid prescribed in various forms, including patches, lozenges, and injections, depending on the patient’s needs.
For chronic pain, transdermal patches provide long-term relief, while lozenges help manage breakthrough pain in cancer patients. In hospitals, fentanyl injections are commonly used for post-surgical pain and anesthesia.
According to Health Direct, these controlled medical applications help patients with extreme pain conditions when other treatments are insufficient.
How Is Fentanyl Administered in Medical Settings?
Fentanyl is administered in medical settings through intravenous (IV) injection, transdermal patches, lozenges, and nasal spray, depending on the patient’s condition and pain management needs. Each method is designed for specific situations, ensuring controlled and effective relief for severe pain, breakthrough pain, or post-surgical pain.
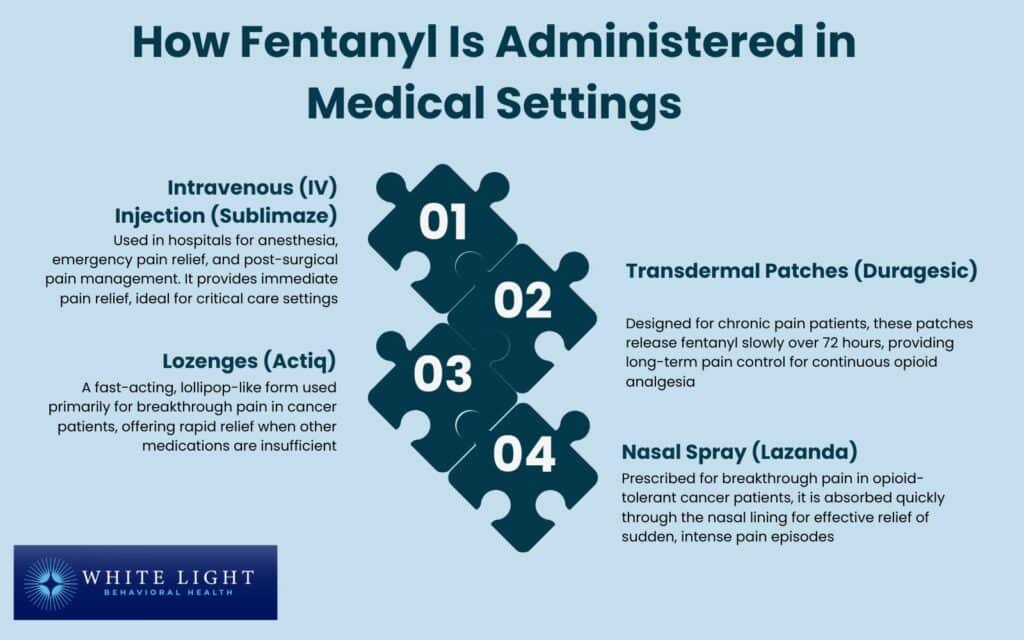
Fentanyl is administered in medical settings in the following ways:
- Intravenous (IV) Injection (Sublimaze): Intravenous (IV) injection is fentanyl is used in hospitals for anesthesia, emergency pain relief, and post-surgical pain management. IV fentanyl provides immediate effects, making it ideal for critical care settings.
- Transdermal Patches (Duragesic): Transdermal patches of fentanyl are designed for chronic pain patients.
These patches slowly release fentanyl over 72 hours, offering long-term pain control without frequent dosing. They are beneficial for patients requiring continuous opioid analgesia.
- Lozenges (Actiq): Lozenges are a fast-acting, lollipop-like form of fentanyl used primarily for breakthrough pain in cancer patients.
It benefits those needing rapid relief when their pain medication is insufficient.
- Nasal Spray (Lazanda): Nasal Spray is prescribed for breakthrough pain in opioid-tolerant cancer patients. This form allows for quick absorption through the nasal lining, making it effective for sudden, intense pain episodes.
What Are the Side Effects of Fentanyl?
The side effects of fentanyl are drowsiness, nausea, confusion, respiratory depression, and constipation, with more severe risks, including addiction and overdose. Short-term side effects include dizziness, sedation, and slowed breathing, which is life-threatening at high doses.
Long-term use of fentanyl, especially with prolonged prescription or misuse, leads to tolerance, dependence, and withdrawal symptoms. According to FDA warnings and clinical trials, fentanyl carries a high risk of respiratory failure, making careful medical supervision necessary for safe use.
What Are the Short-Term Effects of Fentanyl Use?
The short-term effects of fentanyl use are drowsiness, euphoria, nausea, confusion, and slowed breathing, along with dizziness, sedation, and constipation. These effects occur because fentanyl binds to opioid receptors in the brain, altering pain perception and producing a sedative-like state. While some effects are mild, other effects, such as respiratory depression, are life-threatening, especially with misuse or overdose.
According to Sloan PA et al. 1998 in “A Clinical Evaluation of Transdermal Therapeutic System Fentanyl for the Treatment of Cancer Pain,” 30% of patients reported adverse effects from the fentanyl patch. The most common side effects included nausea (13%), vomiting (8%), skin rash (8%), and drowsiness (4%).

The short-term effects of fentanyl use are as follows:
- Slowed Breathing (Respiratory Depression): Respiratory depression is a dangerous reduction in breathing rate caused by fentanyl’s impact on opioid receptors in the brainstem, which leads to oxygen deprivation, coma, or death in high doses. As studied by Topacoglu H, Karcioglu O, Cimrin AH, Arnold J., et al. 2005 in the case study titled “Respiratory Arrest After Low-Dose Fentanyl,” fentanyl use causes hypoventilation, respiratory distress, and oxygen deprivation, which progress to respiratory failure, a major cause of fentanyl-related deaths.
This physical side effect directly impacts lung function and the body’s ability to absorb oxygen.
- Drowsiness: Drowsiness is the state of extreme tiredness caused by fentanyl’s depressant effects on the central nervous system (CNS). Fentanyl slows brain activity and reduces alertness in most users.
- Euphoria: Euphoria is the feeling of intense happiness due to fentanyl triggering the dopamine release in the brain.
This reinforces drug-seeking behavior and increases the risk of addiction.
- Nausea and Vomiting: Nausea and vomiting are common side effects caused by fentanyl’s effect on the brainstem, which controls nausea and vomiting responses, leading to discomfort and potential dehydration.
- Confusion: A cognitive impairment resulting from fentanyl’s suppression of brain function, affecting memory, concentration, and decision-making abilities. A study by Tamargo JA MS et al. 2021 in “Cognitive Impairment among People Who Use Heroin and Fentanyl: Findings from the Miami Adult Studies on HIV (MASH) Cohort,” found that cognitive impairment was more prevalent in individuals using heroin and/or fentanyl compared to those misusing prescription opioids, with rates of 31.6% versus 10.5%.
Contact us today to schedule an initial assessment or to learn more about our services.
Whether you are seeking intensive outpatient care or simply need guidance on your mental health journey, we are here to help.
What Are the Long-Term Health Risks of Fentanyl Use?
The long-term health risks of fentanyl use are dependence, respiratory issues, immune suppression, cognitive decline, and opioid-induced hyperalgesia. Chronic fentanyl use alters brain chemistry, weakens the body’s ability to fight infections, and increases sensitivity to pain over time. These risks make long-term fentanyl use particularly dangerous, even when taken as prescribed.
The long-term effects of fentanyl use are as follows:
- Dependence: A physical and psychological reliance on fentanyl due to repeated activation of opioid receptors, leading to withdrawal symptoms when use is reduced or stopped. Research published in Nature indicates that fentanyl poses a greater risk of abuse compared to other opioids, largely due to its rapid onset and strong reinforcing effects.
A study by Alzu’bi A. et al. 2024, titled “The Impact of Chronic Fentanyl Administration on the Cerebral Cortex in Mice: Molecular and Histological Effects” highlights how fentanyl influences behavior and psychology by affecting mood, intensifying cravings, and driving compulsive drug-seeking behavior.
- Respiratory Issues: Long-term fentanyl use causes persistent respiratory depression, reducing lung function and increasing the risk of hypoxia (oxygen deficiency), which leads to organ damage. According to a study by Solis E Jr, Cameron-Burr KT, Shaham Y, and Kiyatkin EA. et al. 2018, titled “Fentanyl-Induced Brain Hypoxia Triggers Brain Hyperglycemia and Biphasic Changes in Brain Temperature,” this physical side effect of fentanyl leads to unconsciousness or even death.
- Immune Suppression: Chronic opioid use weakens the immune system by altering white blood cell activity, making individuals more susceptible to infections and illnesses.
- Cognitive Decline: Long-term fentanyl exposure impairs memory, attention, and executive functioning due to changes in neurotransmitter balance, reducing overall cognitive abilities.
- Opioid-Induced Hyperalgesia: Opioid-induced hyperalgesia is a paradoxical condition where prolonged fentanyl use increases pain sensitivity rather than relieving it due to changes in the way pain signals are processed in the nervous system.
How Does Fentanyl Affect the Brain?
Fentanyl affects the brain by binding to opioid receptors in the central nervous system, blocking pain signals and triggering a surge in dopamine release, which creates intense feelings of euphoria and relaxation.
This process reinforces drug-seeking behavior and increases the risk of addiction. According to a neuroscientific study by Solis E Jr, Cameron-Burr KT, Shaham Y, Kiyatkin EA. et al. 2018, titled “Fentanyl-Induced Brain Hypoxia Triggers Brain Hyperglycemia and Biphasic Changes in Brain Temperature,” fentanyl is at least 20-fold more potent than heroin in causing brain hypoxia.
Its consumption, either by mistaking it for heroin or as a contaminant of ‘street heroin,’ could result in strong brain hypoxia, with possible lethality.
Prolonged fentanyl use alters neuroplasticity, weakening the brain’s ability to adapt and leading to tolerance, where higher doses are needed to achieve the same effect. Over time, this results in dependence, cognitive impairment, and difficulty regulating emotions, memory, and decision-making. These changes make fentanyl highly addictive and significantly impact brain function.
Can Fentanyl Cause Seizures or Hallucinations?
Yes, fentanyl can, in rare cases, cause seizures and hallucinations, particularly during overdose or long-term use. These neurological side effects occur due to disruptions in brain activity and oxygen deprivation, which lead to abnormal electrical signaling and altered perception. While seizures and hallucinations are uncommon, they occur in a small percentage of users, especially in cases of high-dose fentanyl exposure or withdrawal.
According to Woodhouse A, Ward ME, Mather LE. et al. 1999, titled “Intra-subject variability in post-operative patient-controlled analgesia (PCA): is the patient equally satisfied with morphine, pethidine and fentanyl?” hallucinations have been observed in up to 6% of patients (5 out of 82) receiving fentanyl through patient-controlled intravenous analgesia for acute postoperative pain. Case reports suggest a connection between fentanyl-induced hallucinations and the high doses administered for cancer pain management.
Can Fentanyl Cause a Heart Attack?
Yes, fentanyl can potentially cause a heart attack by lowering blood pressure, slowing heart rate, and reducing oxygen levels, increasing cardiovascular risks. Severe respiratory depression from fentanyl use leads to oxygen deprivation (hypoxia), which strains the heart and triggers a cardiac event. Research indicates that opioid use, including fentanyl, is associated with higher risks of arrhythmias, myocardial infarction, and sudden cardiac arrest, particularly in individuals with pre-existing heart conditions.
A study by Eroglu TE, Barcella CA. et al. 2022, titled “Opioid use is associated with increased out-of-hospital cardiac arrest risk among 40,000 cases across two countries,” found that opioid users had a significantly higher risk of OHCA in both the Netherlands (OR 2.1) and Denmark (OR 1.8). This association was observed across both sexes and individuals with or without preexisting cardiovascular disease. The increased risk stems from fentanyl’s effects on respiratory depression, reduced oxygen levels, and cardiovascular instability, which triggers cardiac events.
How Does Fentanyl Overdose Happen?
Fentanyl overdose happens when the drug slows or stops breathing, leading to oxygen deprivation and potential death. This occurs because fentanyl, a potent opioid, rapidly binds to opioid receptors in the brain, overwhelming the body’s ability to regulate respiration.
According to the CDC, fentanyl is involved in over 70% of opioid-related overdose deaths due to its extreme potency, which is 50 times stronger than heroin. Non-medical use, especially when mixed with other substances, increases the risk of respiratory failure and fatal overdose.
Fentanyl overdose occurs in the following steps:
- Rapid Central Nervous System Depression: Fentanyl quickly binds to opioid receptors, shutting down pain signals and slowing brain activity.
- Respiratory Suppression: The drug depresses the respiratory center in the brainstem, causing shallow or irregular breathing.
- Oxygen Deprivation (Hypoxia): As breathing slows or stops, oxygen levels in the blood drop, leading to confusion, unconsciousness, and potential brain damage.
- Respiratory Failure and Cardiac Arrest: If untreated, lack of oxygen causes the heart to stop, resulting in death. Emergency intervention with naloxone (Narcan) is necessary for reversing the overdose.
Rediscover Life at White Light Behavioral Health
Get the compassionate support you deserve. We're here to help you reclaim joy, wellness, and a brighter future.
Our Facility
What Are the Signs of a Fentanyl Overdose?
The signs of a fentanyl overdose are slow or stopped breathing, pinpoint pupils, unconsciousness, and cold or clammy skin. Other symptoms include extreme drowsiness, blue-tinged lips or fingernails due to lack of oxygen, a weak pulse, and gurgling or choking sounds. As fentanyl suppresses the central nervous system, breathing becomes dangerously slow, leading to respiratory failure, loss of consciousness, and potential death if not treated immediately with naloxone (Narcan).
How Can You Respond to a Fentanyl Overdose?
You can respond to a fentanyl overdose by calling 911 immediately, administering naloxone (Narcan), and performing rescue breathing if the person is not breathing properly. Since fentanyl causes respiratory failure, emergency response is important.
Naloxone, an opioid antagonist, quickly reverses the effects of fentanyl by blocking opioid receptors. It is available as a nasal spray (Narcan) or injection and requires multiple doses due to fentanyl’s potency.
According to the CDC in Clark AK, Wilder CM, Winstanley EL. et al. 2014, titled “A systematic review of community opioid overdose prevention and naloxone distribution programs,” naloxone has been shown to reverse overdoses in 75% to 100% of cases when given in time. Even after revival, medical attention is necessary to prevent complications or re-overdose, as fentanyl remains in the system longer than naloxone’s effects.
How Can Fentanyl Overdose Be Prevented?
Fentanyl overdose can be prevented by using the drug only as prescribed, avoiding illicit fentanyl, and ensuring access to naloxone (Narcan) for emergencies. Since fentanyl is extremely potent, even small amounts cause a fatal overdose, especially when mixed with other substances. Harm reduction strategies, including education, proper medication use, and emergency preparedness, prevent overdose-related deaths.
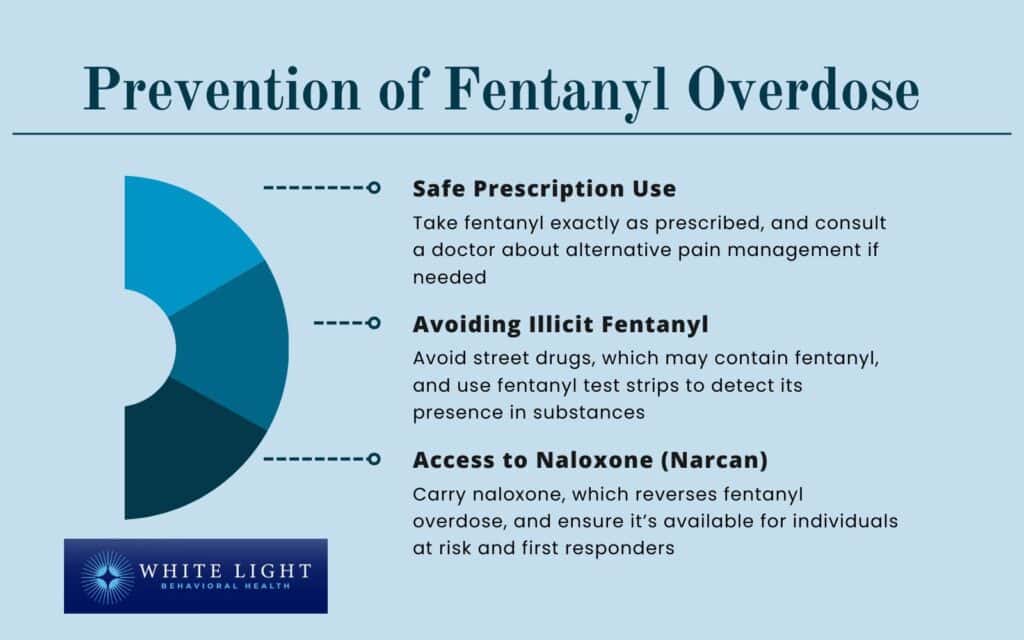
Fentanyl overdose can be prevented in the following ways:
- Safe Prescription Use: Taking fentanyl exactly as prescribed by a healthcare provider reduces the risk of overdose. Patients must follow prescribed doses carefully and consult their doctor about alternative pain management options if they experience side effects or develop tolerance.
- Avoiding Illicit Fentanyl: Many street drugs are laced with fentanyl without the user’s knowledge, significantly increasing the risk of overdose.
Testing substances with fentanyl test strips helps detect its presence, while avoiding non-prescribed opioids altogether is the safest approach.
- Access to Naloxone (Narcan): Naloxone, an opioid antagonist, rapidly reverses fentanyl overdose and saves lives. It is available as a nasal spray or injection and should be carried by individuals at risk of overdose, their loved ones, and first responders.
According to the CDC, expanding naloxone availability has helped reduce opioid-related fatalities.
Can Fentanyl Use Lead to Addiction?
Yes, repeated fentanyl use can lead to addiction due to its high potency and rapid effect on the brain’s opioid receptors. According to the NIH and SAMHSA, fentanyl has a strong potential for addiction, as it quickly induces physical dependence and opioid use disorder (OUD).
Physical dependence occurs when the body adapts to fentanyl, leading to withdrawal symptoms when use stops. Fentanyl addiction involves compulsive drug-seeking behavior despite harmful consequences.
The powerful euphoric effects of fentanyl reinforce repeated use, making it highly addictive.
How Long Does Fentanyl Stay in Your System?
Fentanyl stays in your system for 24 to 72 hours, according to Drugs.com, depending on factors like metabolism, dosage, and method of use. Its half-life ranges from 3 to 12 hours, meaning it takes this long for half of the drug to leave the body. Detection times vary by test: blood tests detect fentanyl for up to 12 hours, urine tests for 24 to 72 hours, and hair tests for up to 90 days. Chronic use or slow metabolism extends its presence, while liver function and hydration levels also impact how quickly fentanyl is cleared from the body.
Are you covered for treatment?
White Light Behavioral Health is an approved provider for Blue Cross Blue Shield and TUFTS, while also accepting many other major insurance carriers.
Is Fentanyl Legal?
Yes, fentanyl is legal in the U.S. but highly regulated. Fentanyl is an FDA-approved, Schedule II drug under the Controlled Substances Act, meaning it has recognized medical uses but a high potential for abuse and dependence.
The DEA strictly controls its prescription and distribution, allowing its use only for treating severe pain, such as in cancer or post-surgical care. Illicit fentanyl is manufactured in clandestine labs and trafficked into the U.S., causing a major driver of opioid-related deaths.
States like Ohio have seen a surge in illegal fentanyl trafficking, contributing to the ongoing opioid crisis.
Over 115 million pills containing illicit fentanyl were seized by law enforcement in 2023, as reported by the National Institute on Drug Abuse (NIDA). According to the public safety alert issued by the DEA, analysis of fentanyl-laced fake prescription pills in 2022 revealed that 6 out of 10 contained a potentially lethal dose, an increase from 2021, when 4 out of 10 were found to be lethal.
The legal classification of fentanyl is as follows:
- Schedule II drug – Legal for medical use with restrictions
- DEA-regulated – Requires a prescription and careful monitoring
- Illegal trafficking – Street fentanyl is unregulated, mixed with other drugs, and highly dangerous
Why Is Illicit Fentanyl So Dangerous?
Illicit fentanyl is extremely dangerous due to its high potency and the unpredictability of its presence in street drugs, leading to a significant increase in overdose deaths. As a synthetic opioid, fentanyl is approximately 50 to 100 times more potent than morphine, meaning even a minuscule amount is lethal. Illegally manufactured fentanyl is mixed with other substances like heroin, cocaine, or counterfeit pills without the user’s knowledge, increasing the risk of accidental overdose. In 2022, synthetic opioids, primarily fentanyl and fentanyl analogs, were involved in approximately 68% of overdose deaths in the United States, as reported by the CDC.
How Common Is Fentanyl in Street Drugs?
Fentanyl is very common in street drugs, as it is mixed with substances like heroin, cocaine, and methamphetamine, frequently without users’ knowledge. This practice heightens the risk of overdose, as individuals unknowingly consume lethal doses. The Drug Enforcement Administration (DEA) has reported a significant rise in the detection of fentanyl in various illicit drugs, underscoring its widespread infiltration into the drug supply.
How Many People Have Died from Fentanyl in the U.S.?
In 2022, approximately 73,838 people in the United States died from fentanyl-related overdoses, according to a report by the National Institute for Drug Abuse (NIDA) titled “Drug Overdose Deaths: Facts and Figures.” This marks a significant increase from previous years, reflecting the escalating opioid crisis.
How Much Fentanyl Is Lethal?
As little as 2 milligrams of fentanyl is considered potentially lethal, according to a study by DEA.gov titled “Facts about Fentanyl.” This minuscule amount underscores the drug’s extreme potency and the high risk of overdose, especially when individuals are unaware of its presence in other substances.
Can Fentanyl Be Absorbed Through the Skin?
Yes, fentanyl can be absorbed through the skin, a method utilized in medical settings via transdermal patches designed for controlled release. However, incidental or casual skin contact with illicit fentanyl is unlikely to cause overdose, as significant absorption requires prolonged exposure. The DEA has addressed concerns regarding accidental skin absorption, indicating that brief contact is not harmful.
Did you know most health insurance plans cover substance use disorder treatment? Check your coverage online now.
What Is the Difference Between Fentanyl and Morphine?
The main difference between fentanyl and morphine is their potency; fentanyl is approximately 50 to 100 times more potent than morphine. Both are opioid analgesics used to manage severe pain, but due to its higher potency, fentanyl requires careful dosing and monitoring to prevent overdose. Fentanyl has a quicker onset and shorter duration of action compared to morphine, making it suitable for specific medical situations but also increasing the risk of misuse and accidental overdose.
How Much Stronger Is Fentanyl Than Oxycodone?
Fentanyl is approximately 50 to 100 times more potent than oxycodone. This significant difference in strength elevates the risk of overdose when fentanyl is used improperly or unknowingly ingested, as even a small amount is lethal.
Is Dilaudid Stronger Than Fentanyl?
No, Dilaudid (hydromorphone) is not stronger than fentanyl. Fentanyl is significantly more potent than hydromorphone, with estimates suggesting it is about 50 to 100 times stronger than morphine, whereas hydromorphone is approximately 5 to 7 times more potent than morphine. This substantial difference necessitates careful dosing and monitoring when using fentanyl to avoid overdose.
What Are Fentanyl Analogs, and Why Are They Risky?
Fentanyl analogs are synthetic derivatives of fentanyl designed to mimic its effects but with varying and unpredictable potencies. Examples include carfentanil, which is approximately 100 times more potent than fentanyl and primarily used as a tranquilizer for large animals. These analogs are risky because their extreme potency increases the likelihood of overdose, and their presence in the illicit drug market goes undetected by users, leading to accidental ingestion of lethal doses.
Share This Post
















