Temazepam/ Restoril Addiction: Signs and Symptoms, Risks, Withdrawal Symptoms, and Treatment
Temazepam addiction emerges when reliance on this Temazepam (Restoril) for its sedative effects spirals into misuse, leading to physical and psychological dependency. While Temazepam effectively aids sleep by calming brain activity, its potent sedative properties also lead to patterns of dependency when misused or taken beyond medical guidelines. This propensity for misuse stems from its fast-acting relief, making it a potential risk for individuals vulnerable to other substances addiction or those seeking to self-medicate for stress or anxiety.
Misuse of Restoril is caused by untreated mental health conditions, attempts at managing chronic sleep disturbances, or recreational use for its euphoric effects. The wide availability of benzodiazepine through prescriptions and illicit sources further exacerbates the risk, particularly for individuals who begin using the drug without professional guidance.
Approximately 75 million prescriptions for BZDs were written in the United States in 2008. The prevalence of BZD use in the general population is 4% to 5%.
Usage increases with age, and women are prescribed BZDs twice as often as men, according to a study by Olfson M et al. 2015, titled “Benzodiazepine use in the United States.”
Key symptoms of Temazepam addiction include escalating tolerance, requiring higher doses to achieve the same effect, withdrawal symptoms such as anxiety or insomnia when usage decreases, and behavioral changes like doctor shopping or secretive use. These warning signs highlight the serious implications of dependency, which affects not only physical health but also emotional stability and daily responsibilities.
Health risks associated with Restoril misuse range from impaired cognitive functioning to severe respiratory depression, especially when combined with alcohol or opioids. A cohort study in North Carolina by Dasgupta N et al., 2016, titled “Cohort study of the impact of high-dose opioid analgesics on overdose mortality,” reported that patients receiving both types of medications had an overdose death rate 10 times higher than those receiving only opioids. Long-term use of Temazepam results in chronic issues such as liver damage or memory deficits, while overdoses carry the potential for life-threatening complications.
The withdrawal process from Temazepam includes symptoms like severe insomnia, tremors, and heightened anxiety. These effects, compounded by the risk of seizures or psychological distress, underscore the urgent need for a medically supervised detox program to ensure safety and manage symptom relief effectively.
Treatment options for Temazepam addiction include a combination of medical and therapeutic interventions. Benzodiazepine tapering, cognitive-behavioral therapies, and support systems like family counseling or sober living programs play integral roles in recovery.
Medication-assisted treatment (MAT) is also utilized to ease withdrawal symptoms and prevent relapse, further improving long-term outcomes. Effective treatment involves a personalized approach and ongoing support for long-term recovery, resulting in 75% of people getting back to normal life after addiction, according to Jones CM et al. 2020, titled “Prevalence and correlates of ever having a substance use problem and substance use recovery status among adults in the United States 2018.”
What is Temazepam/Restoril Addiction?
Temazepam, marketed under the brand name Restoril, is a benzodiazepine primarily prescribed for short-term management of insomnia and anxiety. As a central nervous system depressant, it works by enhancing the effects of a neurotransmitter called GABA, which produces calming effects and helps individuals fall asleep.
However, Restoril abuse occurs when the medication is used outside of its prescribed purpose to achieve feelings of relaxation or euphoria. Over time, this misuse leads to dependence, where the individual feels the need to take the drug regularly, not just for its intended use, but to avoid withdrawal symptoms.
Approximately 75 million prescriptions for BZDs were written in the United States in 2008. The prevalence of BZD use in the general population is 4% to 5%.
Usage increases with age, and women are prescribed BZDs twice as often as men, according to a study by Olfson M et al. 2015, titled “Benzodiazepine use in the United States.”
As the body adapts to the consistent presence of Temazepam, tolerance develops, meaning that higher doses are needed to achieve the same sedative effects. This increase in dosage leads to further abuse, increasing the risk of addiction.
The development of dependence is marked by the need to take the drug to avoid withdrawal symptoms, which include anxiety, insomnia, and seizures. Because of the potential for benzodiazepine addiction, long-term use of Restoril is not recommended, and individuals with a history of substance misuse should be closely monitored while using this medication.
Did you know most health insurance plans cover substance use disorder treatment? Check your coverage online now.
How Does Temazepam Addiction Develop?
Temazepam addiction develops by repeated misuse of the drug, leading to physical and psychological dependence due to its effects on the brain and body. Temazepam addiction begins with prolonged use beyond medical guidelines or recreational use as the individual seeks its calming or euphoric effects. Over time, the brain adapts to the presence of the drug, requiring higher doses to achieve the same effects, a phenomenon known as tolerance.
As tolerance builds, the body becomes physically dependent on Temazepam, meaning that its absence leads to withdrawal symptoms like anxiety, insomnia, and seizures. Psychologically, individuals develop a compulsion to use the drug as a coping mechanism for stress or emotional distress.
Temazepam, like other benzodiazepines, alters the brain’s GABA system, which regulates relaxation and sleep. Prolonged use disrupts this balance, making it increasingly difficult for the individual to function without the drug.
Together, these physical and psychological dependencies create a cycle of addiction that is difficult to break without medical intervention and therapy.
Why is Temazepam Addictive?
Temazepam is addictive because it profoundly influences the brain’s neurotransmitters, particularly gamma-aminobutyric acid (GABA), which plays an important role in calming the nervous system. By enhancing GABA activity, Temazepam produces intense sedation and relaxation, creating a euphoric effect that some individuals find appealing. This effect makes the drug particularly attractive for those seeking relief from anxiety, stress, or insomnia.
Over time, the brain adapts to the frequent presence of Temazepam, producing less natural GABA and becoming reliant on the drug to maintain balance. This adaptation leads to tolerance, requiring higher doses to achieve the same calming or sedative effects.
Additionally, the withdrawal symptoms that occur when the drug is discontinued, such as insomnia, anxiety, and restlessness, drive continued use and dependence. These combined factors—the manipulation of neurotransmitters and the potent sedation—make Temazepam highly addictive.
What are the Common Causes of Temazepam Misuse?
The common causes of Temazepam misuse include mental health challenges, chronic sleep disorders, and self-medication for pain or stress relief. These factors intertwine, making Temazepam misuse a widespread issue for individuals seeking relief from physical or emotional discomfort.

The common causes of Temazepam misuse are as follows:
- Mental Health Challenges: Conditions like anxiety, depression, or post-traumatic stress disorder (PTSD) lead individuals to misuse benzodiazepines like Temazepam for their calming effects. Individuals with anxiety disorders are 2–3 times more likely to misuse prescription medications to manage their symptoms, as Temazepam’s sedative properties provide temporary relief, according to a study by Fluyau D et al. 2024, titled “Temazepam.”
- Chronic Sleep Disorders: Insomnia and other sleep-related problems drive many to misuse Temazepam.
The drug is prescribed for short-term management of sleep difficulties, but prolonged use leads to tolerance and dependence. According to a study by Maust DT et al. 2019, titled “Benzodiazepine Use and Misuse Among Adults in the United States,” nearly 20% of people who misuse benzodiazepines initially start with prescriptions for sleep issues.
- Self-Medication for Pain or Stress Relief: Temazepam misuse stems from attempts to alleviate chronic pain or high-stress levels.
Individuals who lack access to appropriate medical care or who face stigma around mental health treatment turn to Temazepam for self-medication, exacerbating the risk of misuse and addiction.
Who Is at Risk of Restoril Addiction?
The individuals at risk for Restoril addiction include those with certain demographic, psychological, and personal factors that make them vulnerable to dependence. These risks stem from underlying health conditions, life circumstances, or patterns of use.

The groups and factors at higher risk of Restoril addiction are as follows:
- Individuals with Mental Health Disorders: People with conditions like anxiety, depression, or PTSD are more likely to misuse benzodiazepines like Restoril (Temazepam) due to their calming and sedative effects. A study by Schmitz A. et al. 2016, titled “Benzodiazepine use, misuse, and abuse: A review,” suggests that 30–50% of those who misuse prescription drugs have underlying mental health issues.
- People with a History of Substance Abuse: Individuals with prior addiction to alcohol, opioids, or other drugs face an increased risk of dependence on Restoril, according to WebMD in “Restoril – Uses, Side Effects, and More.” A history of addiction correlates with behaviors that heighten the likelihood of misuse.
- Older Adults: Seniors are prescribed Temazepam for sleep issues, but age-related changes in metabolism make them more prone to tolerance and dependence.
Reports by the National Institute of Health in “Benzodiazepine Often Used in Older People Despite Risks” estimate that up to 17% of older adults use benzodiazepines long-term, a known risk factor for addiction.
- Individuals Facing Chronic Stress or Sleep Disorders: Persistent stress, insomnia, or other sleep disturbances drive people to misuse Restoril for its sedative properties. Long-term use to self-medicate leads to addiction.
- Young Adults or Adolescents: Recreational use of benzodiazepines, including Restoril, is more common in younger age groups.
Peer pressure and accessibility of prescription drugs contribute to the rising misuse rates among this demographic.
How Long Does It Take to Become Dependent on Temazepam?
It takes more than 10 days of consistent use to become dependent on Temazepam, especially when taken beyond the prescribed duration or in higher doses, according to the Mayo Clinic. Temazepam, a benzodiazepine, is prescribed for short-term use to treat insomnia.
Prolonged use beyond this recommended 7–10 day period increases the risk of developing dependence, as the brain begins to rely on the drug’s effects to regulate sleep and relaxation. Dependence forms more quickly with higher doses or frequent use because the body builds tolerance, requiring more of the medication to achieve the same effects.
Individuals taking Temazepam for longer than advised experience withdrawal symptoms if they try to stop, which is a hallmark of benzodiazepine dependence. Always follow medical guidance and avoid exceeding the prescribed duration to minimize the risk.
Contact us today to schedule an initial assessment or to learn more about our services. Whether you are seeking intensive outpatient care or simply need guidance on your mental health journey, we are here to help.
What Are the Early Signs of Temazepam Dependency?
The early signs of Temazepam dependency include subtle changes in behavior and physical responses that escalate if unchecked. These signs emerge within the first few weeks of frequent or prolonged use. These signs seem mild initially but progress rapidly into severe benzodiazepine dependence if the medication is not managed under proper medical guidance.
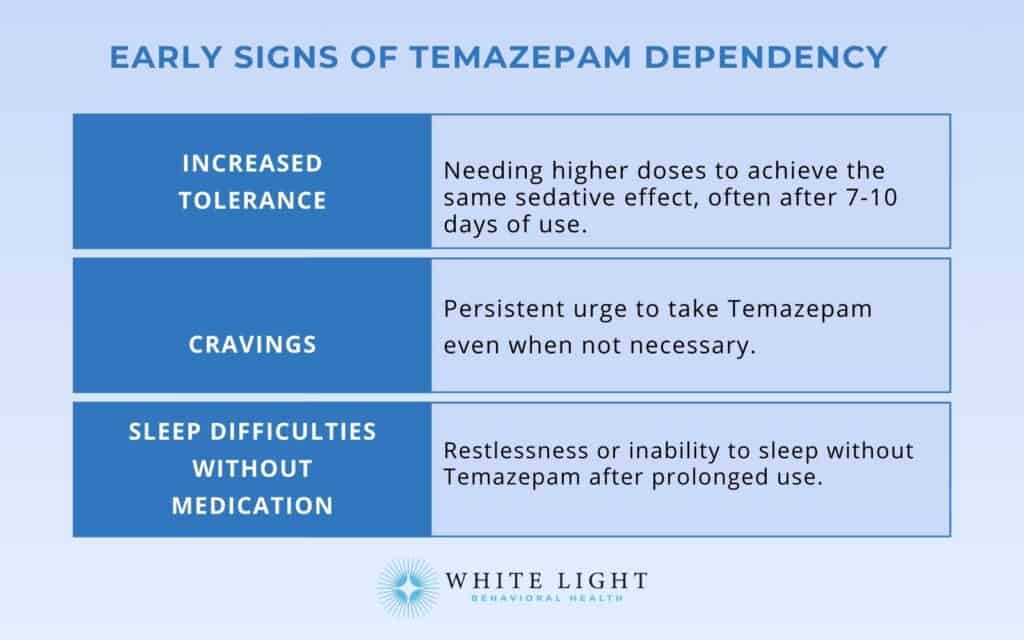
The early signs of Temazepam dependency are as follows:
- Increased Tolerance: Increased tolerance means higher doses of Temazepam are required to achieve the same sedative or sleep-inducing effects. Tolerance is among the early signs of Temazepam dependency, which appear after the recommended use of 7 to 10 days of Restoril use.
This is a strong indicator of the body adapting to the drug.
- Cravings for the Drug: Temazepam craving is experiencing a persistent urge to take medicine outside of prescribed use, even when not necessary for its intended purpose. Cravings start subtly but intensify with continued use.
- Difficulty Sleeping Without the Medication: If an individual continues using Restoril beyond the medically advised 7 to 10 days of use, the body struggles to fall asleep or experiences restlessness on nights without Temazepam.
This indicates that the body has started to rely on the drug and is becoming dependent on Temazepam to fall or stay asleep.
What Are Signs and Symptoms of Temazepam Addiction?
The signs and symptoms of Temazepam addiction include changes in physical health, emotional well-being, and behavior that reflect dependence on the drug. These symptoms worsen over time and affect various aspects of daily life.
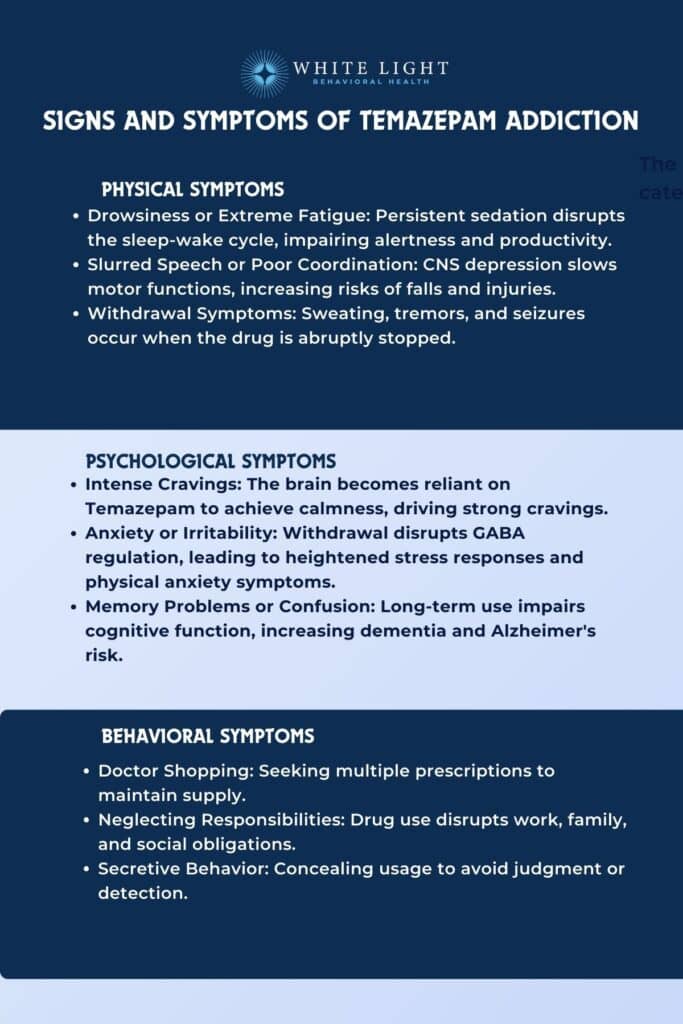
The physical signs of Temazepam addiction are as follows:
- Drowsiness or Extreme Fatigue: Persistent sedation due to overuse of Temazepam disrupts the body’s natural sleep-wake cycle. A study by Edinoff AN et al. 2021, titled “Benzodiazepines: Uses, Dangers, and Clinical Considerations,” has shown that misuse of benzodiazepines like Temazepam impairs alertness and causes excessive fatigue, even after sufficient rest, leading to accidents and reduced productivity.
- Slurred Speech or Poor Coordination: Slurred speech occurs due to Temazepam’s depressive effects on the central nervous system (CNS), which slows down motor functions.
A study by Na I et al. 2022, titled “Risk of Falls Associated with Long-Acting Benzodiazepines or Tricyclic Antidepressants Use in Community-Dwelling Older Adults: A Nationwide Population-Based Case-Crossover Study,” found that prolonged CNS depression increases the risk of falls and injuries, especially in older adults.
- Withdrawal Symptoms: Physical withdrawal symptoms like sweating, tremors, and seizures are well-documented in cases of Temazepam dependence. Approximately 40% of people on benzodiazepines for more than 6 months will have moderate to severe withdrawal, and the remaining 60% will have a relatively mild withdrawal syndrome, according to a study by Hood SD et al. 2014, titled “Benzodiazepine dependence and its treatment with low dose flumazenil.”
The psychological symptoms of Temazepam addiction are as follows:
- Intense Cravings for the Drug: The benzodiazepine mechanism enhances GABA (gamma-aminobutyric acid) neurotransmitter activity, creating a calming effect. Over time, the brain becomes reliant on the drug to achieve this state, leading to cravings.
- Anxiety or Irritability: Temazepam withdrawal disrupts the natural GABA regulation, increasing excitability in the brain.
This leads to heightened stress responses, including physical symptoms such as muscle tension, tight chest, fast heartbeat, sweating, trembling, or shaking, according to Mind in “Withdrawal effects of benzodiazepines.”
- Memory Problems or Confusion: Long-term use impairs cognitive function by reducing hippocampal neurogenesis. A study by Gray SL et al. 2016, titled “Benzodiazepine use and risk of incident dementia or cognitive decline: a prospective population-based study,” examined benzodiazepine use, including Temazepam, found that cumulative exposure to these medications is associated with an increased risk of developing dementia and Alzheimer’s disease.
Over an average follow-up of 7.3 years, 23.2% of participants developed dementia, with 637 cases of Alzheimer’s disease. Low to moderate cumulative use (1-120 standardized daily doses) showed a 25-31% increased risk of dementia compared to non-use.
However, higher use (≥121 TSDDs) did not correlate with faster cognitive decline.
The behavioral symptoms of Temazepam addiction are as follows:
- Doctor Shopping: This behavior is common among those addicted to prescription drugs like Temazepam. According to the National Institute on Drug Abuse (NIDA), approximately 21% of patients who misuse prescription drugs report obtaining them from multiple prescribers.
- Neglecting Responsibilities: Substance abuse frequently disrupts work, family, and social life.
The 2008 NSDUH (National Survey on Drug Use and Health) statistics revealed that approximately 6.2 million individuals aged 12 or older (2.5% of the population) used prescription-type psychotherapeutic drugs non-medically in the past month. Among these non-medical users, 55.9% obtained the drugs for free from a friend or relative, with 81.7% of those friends or relatives having received the medication from a single doctor.
Additionally, 18.0% of non-medical users sourced their prescription drugs from only one doctor.
- Secretive Behavior: Concealing drug use is motivated by guilt or fear of judgment. A study by Maust DT et al. 2019, titled “Benzodiazepine Use and Misuse Among Adults in the United States,” shows that 54% of individuals with benzodiazepine misuse reported lying about their usage to friends or family.
What Are the Risks and Long-Term Effects of Temazepam Addiction?
The risks and long-term effects of Temazepam addiction include overdose, psychological dependency leading to anxiety or depression, and chronic health issues such as cognitive decline and organ damage.
These risks extend beyond the individual’s physical health, affecting mental well-being, relationships, and social functioning. Prolonged misuse also exacerbates the chances of co-occurring substance abuse and further complicates recovery efforts.
The risks and long-term effects of Temazepam addiction are as follows:
Immediate Health Risks
The immediate health risks of Temazepam addiction include the danger of overdose, dangerous interactions with substances like alcohol or opioids, and acute respiratory depression. Overdose risk escalates when Temazepam is combined with other central nervous system depressants, leading to life-threatening complications such as coma or death. For example, a cohort study in North Carolina by Dasgupta Net al. 2016, titled “Cohort study of the impact of high-dose opioid analgesics on overdose mortality,” found that the overdose death rate among patients receiving both types of medications was 10 times higher than among those only receiving opioids.
The immediate health risks of Temazepam addiction are as follows:
- Overdose: Overdose is a significant risk, particularly when combined with alcohol or other sedatives or opioids, leading to slowed breathing and potentially fatal outcomes. According to a report by the Centers for Disease Control and Prevention (CDC) titled “Trends in Nonfatal and Fatal Overdoses Involving Benzodiazepines — 38 States and the District of Columbia, 2019–2020” from 2019 to 2020, benzodiazepine-involved overdose deaths increased significantly, with a 21.8% rise in prescription benzodiazepine deaths with 92.7% among them involved opioids,
- Severe Drowsiness: Severe drowsiness, light-headedness, and confusion are common side effects of Temazepam, as mentioned by GoodRx in “8 Benzodiazepine Side Effects You Should Know About”.
Temazepam’s sedative effects impair motor skills, leading to accidents or injuries.
- Respiratory Depression: High doses of Temazepam suppress breathing, resulting in respiratory depression and respiratory arrest. These effects pose a life-threatening risk, as studied by Vozoris NT et al. 2016, in “Do benzodiazepines contribute to respiratory problems?”
Long-Term Physical and Mental Health Effects
The long-term physical and mental health effects of Temazepam addiction include cognitive decline, persistent mental health disorders like anxiety and depression, and damage to vital organs such as the liver and kidneys.
Chronic use of Temazepam results in memory impairments and reduced ability to perform everyday tasks.
The long-term physical and mental health risks of Temazepam addiction are as follows:
- Cognitive Decline: Long-term Temazepam use results in memory issues and reduced problem-solving abilities, with a heightened risk of dementia. Sustained misuse accelerates age-related cognitive decline, with long-term benzodiazepine use leading to a higher risk of dementia.
A meta-analysis by He Q, Chen X, et al. 2019, titled “Risk of Dementia in Long-Term Benzodiazepine Users: Evidence from a Meta-Analysis of Observational Studies,” pooled ten studies and found that BDZ significantly increases the risk of dementia in the elderly population. This effect was greater in patients using benzodiazepines like Temazepam with a longer half-life (>20 hours half-life) and taking benzodiazepines for more than 3 years.
- Chronic Anxiety and Depression: Temazepam’s prolonged misuse results in worsened psychological health, requiring long-term mental health support, according to WebMD in “Benzodiazepine Abuse.”
- Organ Damage: Liver and kidney damage from prolonged Temazepam processing is well documented.
According to LiverTox: Clinical and Research Information on Drug-Induced Liver Injury, benzodiazepine abuse causes mild serum enzyme elevations and has been linked to only very rare instances of acute, symptomatic liver disease.
Rediscover Life at White Light Behavioral Health
Get the compassionate support you deserve. We're here to help you reclaim joy, wellness, and a brighter future.

What Are the Withdrawal Symptoms of Temazepam?
The withdrawal symptoms of Temazepam include anxiety, tremors, and insomnia. These symptoms are some of the most commonly experienced and range from mild to severe, depending on the duration and dosage of Temazepam use.
Anxiety presents as heightened nervousness or panic attacks, while tremors cause uncontrollable shaking, and insomnia leads to prolonged sleep disturbances. These symptoms reflect the body’s adjustment to the absence of the drug, particularly after developing a physical dependence.
Medical supervision is necessary during Temazepam withdrawal to monitor symptoms and prevent complications. Gradual tapering under a healthcare provider’s guidance is recommended to reduce withdrawal severity and ensure safety.
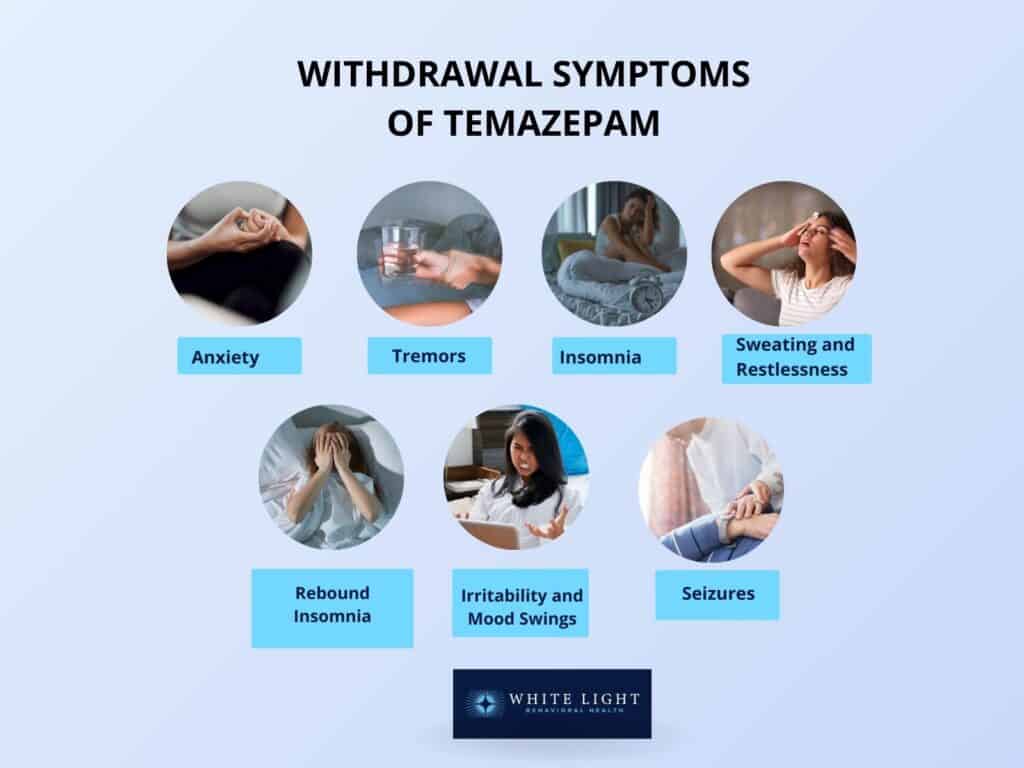
The withdrawal symptoms of Temazepam are as follows:
- Anxiety: Anxiety is characterized by severe nervousness, panic attacks, or a constant feeling of dread. Anxiety is one of the most common psychological withdrawal symptoms.
This begins within 1 to 4 days of discontinuation, depending on the half-life of the Temazepam, according to a study by Pétursson H. et al. 1994, titled “The benzodiazepine withdrawal syndrome.”
- Tremors: Tremors are physical shaking or trembling, usually in the hands, that interferes with daily tasks. They indicate significant withdrawal and escalate if untreated.
- Insomnia: Insomnia is persistent difficulty falling or staying asleep.
As the body struggles to regulate its natural sleep cycle without the sedative effects of Temazepam, it experiences mild to severe insomnia.
- Sweating and Restlessness: Physical restlessness and excessive sweating also occur as the body reacts to Temazepam’s sudden absence.
- Rebound Insomnia: A more severe form of insomnia is called rebound insomnia, which persists for days to weeks and is worse than before starting the medication.
- Irritability and Mood Swings: Emotional instability, including anger, frustration, and sudden mood changes, also appear during the Temazepam withdrawal period.
- Seizures (in severe cases): In cases of long-term or high-dose use of Temazepam, abrupt discontinuation leads to life-threatening seizures, requiring immediate medical attention.
Does Temazepam Need to Be Weaned?
Yes, Temazepam needs to be weaned because abrupt discontinuation of Temazepam leads to severe withdrawal symptoms, including anxiety, insomnia, tremors, and, in extreme cases, life-threatening seizures. Gradually tapering the dosage under medical supervision allows the body to adjust slowly, minimizing the risk of complications and making the withdrawal process safer and more manageable.
According to a study by Morin CM, Bélanger L, Bastien C, Vallières A., et al. 2005, “Long-term outcome after discontinuation of benzodiazepines for insomnia: a survival analysis of relapse,” after 24 months, the relapse rate was significantly lower for those using tapering (30.8%) compared to those in the CBT group (69.2%). Tapering extended the average time to relapse to 18.6 months, making it a more effective approach for long-term benzodiazepine addiction treatment.
How Long Do Withdrawal Symptoms from Temazepam Last?
The withdrawal symptoms from Temazepam last for approximately 2 to 4 weeks, depending on the dosage, duration of use, and individual factors, according to GoodRx in “Benzo Withdrawal Symptoms: What Are They and How Long Do They Last?” Acute symptoms, such as anxiety and insomnia, peak within the first 5 to 10 days, while lingering effects like mood disturbances or mild cravings persist for several weeks. Healthcare professionals recommend a gradual tapering of the dosage to mitigate withdrawal symptoms. This involves reducing the dosage by 25-30 percent initially and then continuing with a 5-10 percent reduction daily or weekly.
How to Manage Temazepam Withdrawal Safely?
To manage Temazepam withdrawal safely, gradual tapering off under professional supervision is recommended. Employing coping strategies is also helpful in managing anxiety and depression experienced during the withdrawal phase.
To manage Temazepam withdrawal safely, the following approaches are recommended:
- Tapering Off Gradually: A slow reduction in dosage under medical supervision helps minimize withdrawal severity and ensures symptom relief. Abrupt cessation triggers severe symptoms like seizures or extreme anxiety.
- Professional Support: Engaging with healthcare providers ensures access to treatments like alternative medications to ease symptoms and monitor potential complications.
Residential detox programs provide a structured environment for recovery.
- Coping Strategies: Employing stress-management techniques such as mindfulness, counseling, and peer support groups address psychological dependence and reinforce long-term sobriety.
Is Medical Supervision Necessary During Temazepam Withdrawal?
Yes, medical supervision is necessary during Temazepam withdrawal because the process involves severe symptoms such as seizures, extreme anxiety, and insomnia, which become life-threatening without professional care. A healthcare provider implements a controlled tapering schedule and provides medications for symptom relief, ensuring safety and comfort throughout withdrawal.
What Are the Treatment Options for Temazepam Addiction?
The treatment options for Temazepam addiction include inpatient and outpatient rehabilitation programs, behavioral therapies, and medication-assisted treatment (MAT), all designed to address the physical and psychological dependence on the drug. These approaches work together to support individuals in achieving recovery and preventing relapse. Effective treatment involves a personalized approach and ongoing support for long-term recovery, resulting in 75% of people getting back to normal life after addiction, according to Jones CM et al. 2020, titled “Prevalence and correlates of ever having a substance use problem and substance use recovery status among adults in the United States 2018.”
The treatment options for Temazepam addiction are as follows:
Are you covered for treatment?
White Light Behavioral Health is an approved provider for Blue Cross Blue Shield and TUFTS, while also accepting many other major insurance carriers.
Check Coverage Now!1. Inpatient and Outpatient Rehabilitation Programs
Inpatient and outpatient rehabilitation programs are structured treatments designed to help individuals recover from Temazepam addiction. Inpatient programs involve staying in a controlled facility, which is particularly effective for severe cases or when withdrawal symptoms are acute. Outpatient programs, on the other hand, allow individuals to live at home while attending therapy sessions and receive medical care while continuing their daily activities.
Inpatient is Compared to the Outpatient Rehabilitation Programs as Follows:
- Inpatient Programs: Inpatient rehabilitation programs require full-time residency in a treatment center. They offer 24/7 medical supervision and support and are most effective for severe dependencies or co-occurring conditions.
According to a study by Greenfield L et al. 2004, titled “Effectiveness of long-term residential substance abuse treatment for women: findings from three national studies,” clients who stayed in inpatient treatment for at least 3 months and achieved their treatment goals had an abstinence rate of 76%-78%, similar to those who stayed longer than 6 months.
- Outpatient Programs: Outpatient programs allow patients to remain at home while attending scheduled sessions. It is suitable for mild-to-moderate addiction cases and is more affordable and flexible than inpatient rehab programs, but it requires strong personal commitment.
A study published in the Journal of Substance Abuse Treatment, titled “ Substance Abuse Intensive Outpatient Programs: Assessing the Evidence,” found that individuals who completed an IOP achieved similar rates of abstinence and reductions in substance use compared to those who completed residential treatment. IOPs offer a significant benefit for those unable to commit to inpatient care while maintaining strong effectiveness, with success rates for IOP participants falling between 50% and 70%.
2.
Behavioral Therapies
Behavioral therapies focus on addressing the underlying behaviors and thought patterns associated with Temazepam addiction. These therapies are important for identifying triggers and building resilience against relapse.
The common behavioral therapies to treat Temazepam addiction are as follows:
- Cognitive Behavioral Therapy (CBT): CBT is a psychological treatment that helps individuals identify and change negative thought patterns and behaviors linked to addiction. CBT reduces substance use by 60%-70% when combined with other treatments, according to a study by Otto MW, McHugh RK, Simon NM, Farach FJ, Worthington JJ, and Pollack MH. et al. 2010, “Efficacy of CBT for benzodiazepine discontinuation in patients with panic disorder: Further evaluation.”
- Dialectical Behavioral Therapy (DBT): DBT focuses on emotional regulation and mindfulness to prevent impulsive drug use.
Particularly effective for individuals with co-occurring mental health disorders. In one study, 96% of DBT participants completed all sessions, compared to 77% of control group participants, according to a survey by Davoudi M et al. 2021, titled “A pilot randomized controlled trial of dialectical behavior therapy (DBT) for reducing craving and achieving cessation in patients with marijuana use disorder: feasibility, acceptability, and appropriateness.”
- Group Counseling: Group counseling provides peer support and shared experiences to reduce feelings of isolation.
It encourages accountability and has been shown to increase long-term recovery rates by 20%, according to a study by Wendt DC and Gone JP. et al. 2017, titled “Group Therapy for Substance Use Disorders: A Survey of Clinician Practices.”
3. Medication-Assisted Treatment (MAT)
Medication-assisted treatment (MAT) uses FDA-approved medications to alleviate withdrawal symptoms and reduce cravings during recovery.
MAT is particularly useful for managing the physical dependency associated with Temazepam. For example, drugs like flumazenil are used under supervision to manage severe benzodiazepine dependence.
Medications are combined with therapy to ensure long-term recovery. According to a 2013 study, ” Management of Benzodiazepines in Medication-Assisted Treatment, ” MAT increases treatment retention rates by 50%- 70%, with reduced relapse rates compared to non-MAT approaches.
Adjunct medications address co-occurring disorders, enhancing the effectiveness of the overall treatment plan.
4. Support Systems and Aftercare
Support groups and aftercare services are necessary to maintain recovery after initial treatment.
Support groups like 12-step programs or local addiction recovery communities provide a network of individuals with shared experiences. Family therapy and ongoing counseling address relational dynamics and build a supportive environment for the recovering individual.
Aftercare programs, including routine check-ins and continued therapy, are designed to reduce the risk of relapse. Consistent aftercare participation lowers relapse rates by up to 40%, according to a study by Finney J, Moos R, Timko C., et al. 1999, “The course of treated and untreated substance use disorders: remission and resolution, relapse and mortality.”
How to Prevent Relapse from Restoril Addiction?
To prevent relapse from Restoril addiction, it is important to employ effective strategies that focus on both psychological and lifestyle changes to maintain sobriety. Preventing relapse involves not just stopping drug use but also addressing the underlying factors that contributed to addiction in the first place. Developing coping mechanisms for stress and temptation, along with building a strong support system, is necessary for long-term recovery.
To prevent relapse from Restoril addiction, the following strategies are employed:
- Coping Skills Development: Learning and practicing coping mechanisms for stress, anxiety, or triggers that lead to temptation, such as mindfulness, deep breathing exercises, or cognitive behavioral techniques (CBT).
- Engagement in Sober Living: Establishing a lifestyle that supports sobriety, such as joining sober living communities, where individuals live in an alcohol—and drug-free environment and offer support and accountability during the recovery process.
- Therapy and Counseling: Regular therapy sessions, such as individual or group counseling, focus on both the psychological aspects of addiction and developing strategies for managing cravings and maintaining sobriety.
- Building a Support System: Surrounding oneself with a supportive network of family, friends, or support groups such as 12-step programs (e.g., Narcotics Anonymous) that provide motivation and encouragement during recovery.
Did you know most health insurance plans cover substance use disorder treatment? Check your coverage online now.
What Are Strategies for Building Long-Term Recovery From Temazepam Addiction?
The strategies for building long-term recovery from Temazepam addiction include developing personal goals, maintaining a strong support network, and incorporating healthy lifestyle changes. Long-term recovery is a continuous process that requires consistent effort, emotional resilience, and a commitment to personal growth. By integrating these strategies into daily life, individuals sustain sobriety, reduce relapse risk, and improve overall well-being.
The strategies for building long-term recovery from Temazepam addiction are as follows:
- Setting Personal Goals: Establishing clear, achievable goals helps individuals focus on their recovery and maintain motivation. These goals relate to personal health, career, or relationships and provide a structured way to track progress over time.
- Building and Maintaining a Support Network: It is important to stay connected with others who understand the challenges of recovery.
Support groups such as 12-step programs (e.g., Narcotics Anonymous), therapy groups, and family members offer important emotional support. A strong network provides encouragement and accountability, which significantly reduces the likelihood of relapse.
- Incorporating Healthy Lifestyle Changes: Adopting a balanced lifestyle through exercise, proper nutrition, and stress management techniques (like yoga or mindfulness) enhances physical and mental well-being.
These changes not only support sobriety but also improve the overall quality of life, reducing the temptation to return to old habits.
How Does Temazepam Addiction Compare to Other Substance Addictions?
Temazepam addiction is compared to other substance addictions based on its effects, dependency potential, and withdrawal symptoms. Temazepam, a benzodiazepine, is commonly prescribed for anxiety and insomnia.
Like other benzodiazepines and sedative-hypnotic drugs, it carries risks of dependency, misuse, and withdrawal, but its addictive potential and severity of withdrawal symptoms differ based on the specific substance and individual usage patterns.
The comparison of Temazepam addiction to other substance addictions is as follows:
- Diazepam (Valium): Diazepam is another benzodiazepine used to treat anxiety and muscle spasms. It shares similar dependency risks with Temazepam but has a longer half-life, meaning it stays in the body longer.
This results in a slightly slower development of dependency but increases withdrawal duration when cessation occurs. Withdrawal symptoms are severe and similar to those of Temazepam.
According to the report by the Substance Abuse and Mental Health Services Administration. (2021, titled “Key substance use and mental health indicators in the United States: Results from the 2020 National Survey on Drug Use and Health,” approximately 971,000 people aged 12 or older misused diazepam (Valium) in the past year.
Researchers estimate that around 2% of people who use benzodiazepines like diazepam eventually develop an addiction.
- Lorazepam (Ativan): Lorazepam is used to manage anxiety and insomnia. Like Temazepam, it has a high potential for misuse, and the withdrawal process is similarly challenging, with symptoms including agitation and seizures.
Lorazepam, however, has a shorter half-life, which means it acts more quickly but also increases the risk of dependency in people who take it frequently. In 2019, pharmacists in the United States filled an estimated 92 million benzodiazepine prescriptions—20% of which were scripts for lorazepam, according to the U.S. Food and Drug Administration 2020, “FDA requiring labeling changes for benzodiazepines.”
- Alprazolam (Xanax): Alprazolam is known for its quick onset and high potency.
It has a stronger potential for addiction compared to Temazepam, especially in those who use it for long periods. Withdrawal from Alprazolam is more intense and involves panic attacks, which is a significant difference from the more gradual withdrawal of Temazepam.
In 2020, 1.2% of people aged 12 and older misused Xanax, according to a study by the Substance Abuse and Mental Health Services Administration titled “Any use and misuse of sedative subtypes in the past year.”
- Clonazepam (Klonopin): Used to treat panic disorders and seizures, Clonazepam shares many characteristics with Temazepam in terms of dependency potential. However, it is prescribed for longer periods, which leads to a stronger physical dependency.
Withdrawal from Clonazepam is also known to be difficult and mirrors that of Temazepam, but it lasts longer due to its prolonged action. In 2020, approximately 6.2 million individuals in the United States misused tranquilizers or sedatives, including clonazepam.
Misuse of Klonopin was most prevalent among young adults aged 18 to 25, with adults aged 26 and older following closely behind, according to a study by the Substance Abuse and Mental Health Services Administration titled “Key substance use and mental health indicators in the United States: Results from the 2020 National Survey on Drug Use and Health.”
- Zolpidem (Ambien): Zolpidem is a non-benzodiazepine sedative used for insomnia. While it has a lower risk of dependency than Temazepam, it still carries the potential for misuse, especially in individuals with a history of addiction.
Zolpidem’s withdrawal symptoms tend to be less severe than those of Temazepam but still be unpleasant for frequent users. According to the National Survey on Drug Use and Health, nearly 5 million people over the age of 12 misused prescription tranquilizers or sedatives, like Ambien, in 2022.
- Zopiclone (Imovane): Zopiclone is another sedative-hypnotic drug used for insomnia.
Like Temazepam, Zopiclone leads to dependency and withdrawal symptoms, but it is considered to have a lower risk of addiction compared to benzodiazepines. Its effects on sleep and dependency are similar, but the withdrawal period is shorter.
- Phenobarbital: A barbiturate used for seizure control, Phenobarbital has a higher addiction potential than Temazepam due to its long-acting sedative effects.
Withdrawal from Phenobarbital is more dangerous and causes severe symptoms such as delirium and seizures, which are life-threatening. In contrast, Temazepam withdrawal is less severe but still requires medical supervision.
According to the Substance Abuse and Mental Health Services Administration (SAMHSA), over 52 million Americans aged 12 and older have misused prescription phenobarbital at some point.
- Phenazepam: A benzodiazepine similar to Temazepam, Phenazepam is not widely available in some regions but is used to treat anxiety and sleep disorders. Its addictive potential is higher than that of Temazepam, and its withdrawal symptoms are more intense due to its potency and long half-life.
- Eszopiclone (Lunesta): Used for insomnia, Eszopiclone has a lower dependency risk than Temazepam but still leads to misuse, particularly when taken in higher doses or for extended periods.
Withdrawal symptoms are milder compared to those of Temazepam but include rebound insomnia and irritability. Over 31 million prescriptions for Lunesta have been written since the drug hit the market in 2004, according to a report by the Centers for Disease Control and Prevention (CDC), and nearly 9 million people use prescription sleep aids like Lunesta.
- Triazolam (Halcion): Like Temazepam, Triazolam is used for short-term treatment of insomnia.
It has a very short half-life, which increases the risk of dependency in those who use it for extended periods. Withdrawal from Triazolam includes anxiety and agitation, though the duration of symptoms is generally shorter than Temazepam.
Share This Post
















