What Is Percocet? Definition, Usage, Effects, Addiction

Percocet is a Schedule II controlled substance that contains oxycodone, a potent opioid, and acetaminophen, a non-opioid pain reliever. The Drug Enforcement Administration (DEA) classifies it as a high-risk prescription medication due to its latency for misuse and addiction. In the U.S., opioid prescriptions, including Percocet, contributed to a rise in opioid addiction, with over 2.1 million Americans suffering from opioid use disorder (OUD) in 2021, according to the National Institute on Drug Abuse (NIDA).
Percocet is primarily used for short-term pain relief, especially after surgery, injury, or medical procedures. Percocet is prescribed when non-opioid medications are insufficient, but due to its addictive properties, it is recommended for limited use under strict medical supervision. The Centers for Disease Control (CDC) records that in 2023, approximately 125 million opioid prescriptions, including Percocet, were dispensed to American patients.
Percocet’s effects range from pain relief to sedation and euphoria, including nausea, dizziness, and constipation, while serious risks involve respiratory depression, liver toxicity, and overdose. Combining Percocet with other central nervous system depressants, such as alcohol, increases the likelihood of life-threatening complications. The national opioid dispensing rate steadily declined from 46.8 prescriptions per 100 people in 2019 to 37.5 prescriptions per 100 people in 2023, as provided by the CDC (2024).
Percocet has high addiction potential, as oxycodone binds to opioid receptors in the brain, leading to tolerance and dependence. Long-term use increases the risk of opioid use disorder (OUD), with many individuals transitioning to stronger opioids like heroin or fentanyl. The rise in opioid-related overdoses in the U.S. highlights the dangers of Percocet misuse and the need for strict prescribing practices.
What Is Percocet?
Percocet is a prescription pain reliever that combines oxycodone, a powerful opioid, with acetaminophen, a non-opioid analgesic that enhances pain relief. As a Schedule II controlled substance under the DEA, Percocet is recognized for its medical use but carries a high risk of abuse, dependence, and addiction. Percocet is prescribed for moderate to severe pain management, but its potency and addictive properties make it subject to strict regulations.
Based on combined data from the 2013 and 2014 National Survey on Drug Use and Health (NSDUH), an annual average of 10.7 million people aged 12 or older misused prescription pain relievers in the past year. Nearly half of those who misused these pain relievers reported obtaining them for free from a friend or relative (50.5 percent), while 22.1 percent obtained them from a single doctor.
Did you know most health insurance plans cover substance use disorder treatment? Check your coverage online now.
Is Percocet the Same as Oxycodone?
No, Percocet is not the same as pure oxycodone medications. While oxycodone is a stronger opioid, Percocet contains acetaminophen, which enhances pain relief but intensifies the risk of liver damage.
Unlike extended-release oxycodone, Percocet is an immediate-release medication used for short-term pain management. In fiscal year 2023, the United States Sentencing Commission recorded 64,124 reported cases, with 19,066 involving drugs.
Among these, 18,939 cases were related to drug trafficking, and 1.2% involved oxycodone, marking a 46.4% decline since 2019.
More Resources on Addiction:

What Are the Street Names of Percocet?
The street names of Percocet are oxy, percs, roxy, and Hillbilly heroin. Illicit use of Percocet is dangerous due to unknown dosages, contamination with fentanyl, and an elevated overdose risk.
Percocet is hazardous because it brings addiction, overdose, and serious health risks, such as liver damage and respiratory failure, owing to the combination of oxycodone and acetaminophen.
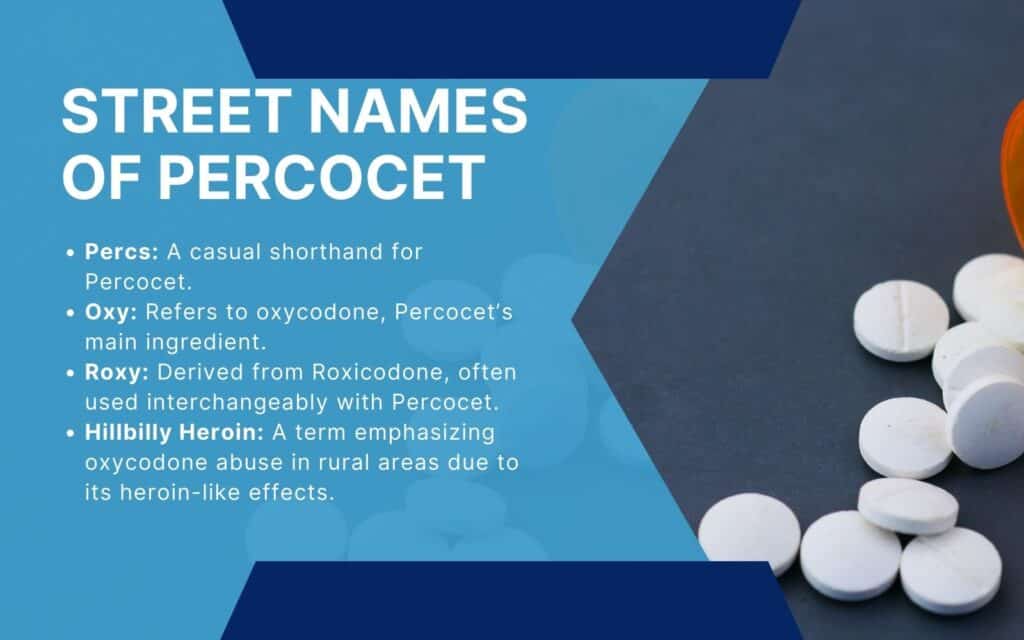
Common street names of Percocet are explained below:
- Percs: A shorthand term for Percocet, used in casual conversations within drug-using communities.
- Oxy: Refers to oxycodone, the main active ingredient in Percocet, and is used to describe any oxycodone-containing medication.
- Roxy: Short for Roxicodone, a form of oxycodone that is sometimes used interchangeably with Percocet in illicit contexts.
- Hillbilly Heroin: A derogatory term that highlights the abuse of oxycodone, particularly in rural areas, due to its opioid-like effects similar to heroin.
How Does Percocet Work?
Percocet works by binding to opioid receptors in the central nervous system, blocking pain signals to the brain. Oxycodone activates mu-opioid receptors, catalyzing analgesia, sedation, and euphoria, while acetaminophen reduces pain through different pathways.
Lambert D. 2023 explores opioid pharmacology, emphasizing its role in pain management and the mechanisms underlying both therapeutic effects and side effects like tolerance and opioid-use disorder. While µ-opioid (MOP) receptors are the primary targets, δ (DOP) and κ (KOP) receptors also contribute to analgesia.
Emerging research on the NOP receptor, which is naloxone-insensitive, leads to safer opioid drugs.
Advances in biased agonism and allosteric modulation (these are new methods in drug development that help make medications work effectively while reducing harmful side effects) offer the capacity for minimizing side effects while maintaining efficacy. The paper also highlights epigenetic links to pain and addiction. Lambert warns against overcorrecting for the opioid crisis, as it does limit access to essential pain relief, particularly in low-income countries as detailed in “Opioids and Opioid Receptors; Understanding Pharmacological Mechanisms As A Key to Therapeutic Advances and Mitigation of the Misuse Crisis.”
What Conditions Is Percocet Used to Treat?
Conditions that Percocet is used to treat are moderate to severe pain, post-surgical pain, and injury-related pain. Percocet is prescribed for short-term pain management because of its likelihood to precipitate addiction and dependence.
Percocet combines oxycodone, a potent opioid, with acetaminophen, which enhances its pain-relieving effects. This amalgamation makes it efficacious for tackling acute pain, such as after surgery or from injuries, but it is not recommended for long-term use attributable to the risks associated with opioids.
How Long Does It Take for Percocet to Kick In?
It takes about 30 to 60 minutes for Percocet to kick in, with the onset time varying depending on factors like the individual’s metabolism and whether it’s taken with food. The absorption rate is influenced by stomach contents, which delay its imposition.
The drug reaches its peak effect around 1 to 2 hours after ingestion. Taking more doses too soon augments the risk of overdose, as the body has not fully processed the initial dose.
Always follow prescribed guidelines to avoid grave health risks.
Contact us today to schedule an initial assessment or to learn more about our services. Whether you are seeking intensive outpatient care or simply need guidance on your mental health journey, we are here to help.
What Are the Dangers of Taking Percocet?
The dangers of taking Percocet are addiction, overdose, and a range of common and serious side effects, even when taken as prescribed like nausea, dizziness, constipation, drowsiness, e respiratory depression, and liver damage (due to the acetaminophen). The addiction risk is huge due to the oxycodone component, which encourages physical dependence over time.
Overdose concerns are heightened, as misuse or taking too many doses too soon results in life-threatening respiratory failure. The U.S. has seen a dramatic rise in opioid crisis deaths, with Percocet-related overdose contributing to the alarming statistics.
In 2019, approximately 600,000 deaths worldwide were attributed to drug use, with nearly 80% of these fatalities linked to opioids. Of these, about 25% were caused by opioid overdose, according to the World Health Organization (2023).
What Are the Common Side Effects of Percocet?
Common side effects of Percocet comprise drowsiness, nausea, constipation, dizziness, and headaches. These side effects underscore the importance of careful monitoring when using Percocet, especially with prolonged or higher doses. Frequent adverse reactions of Percocet affect more than 5% of patients, encompassing asthenia, constipation, dizziness, dry mouth, headache, nausea, pruritus, somnolence, sweating, and vomiting, as noted by Sadiq et al. 2023 in “Oxycodone.”
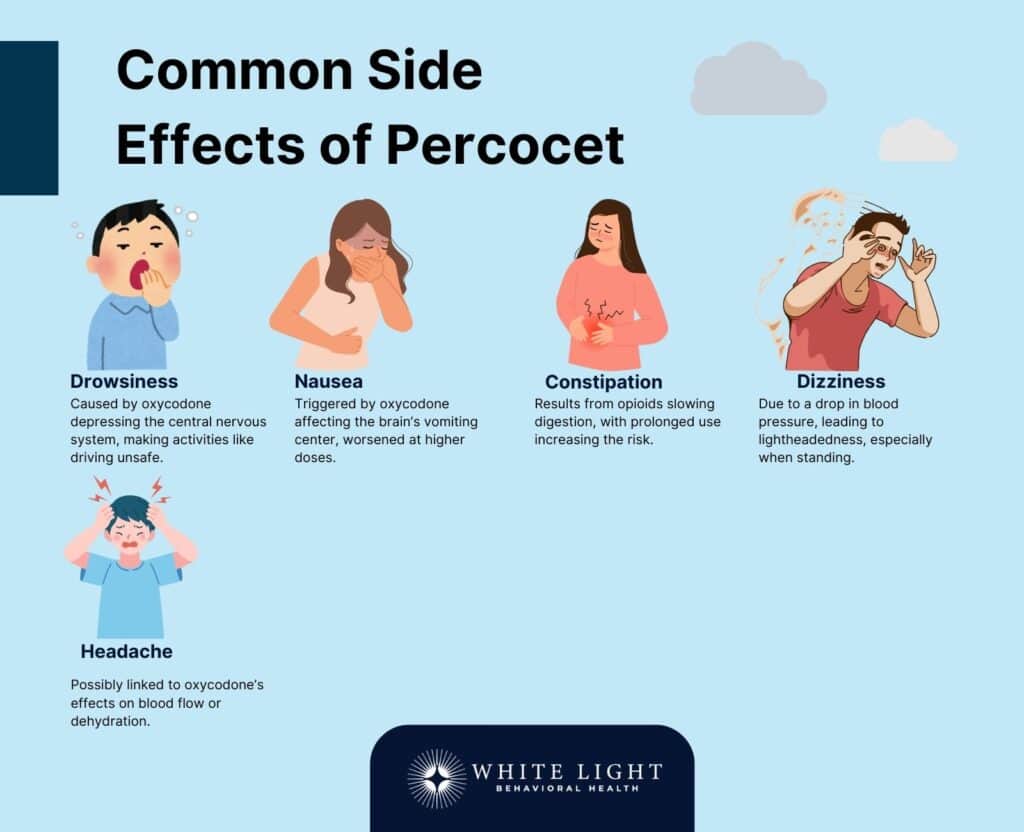
The most common side effects are given below:
- Drowsiness: Drowsiness is a feeling of tiredness or lethargy. This occurs because oxycodone, the opioid in Percocet, depresses the central nervous system, enkindling sedation.
This side effect interrupts activities like driving or operating machinery.
- Nausea: An upset stomach or feeling of sickness. Opioids like oxycodone trigger the brain’s vomiting center, leading to gastrointestinal discomfort.
Users experience nausea, which is worse at higher doses or when starting treatment.
- Constipation: Difficulty in passing stools, caused by the way opioids slow down the digestive system. Percocet, with its oxycodone content, vitiates gut motility, setting off constipation.
Ducrotté et al. 2016 investigated the prevalence and clinical features of opioid-induced constipation (OIC) in France through a survey of 15,213 individuals.
Among the 31.2% who reported opioid use, 8.7% experienced OIC, with the prevalence rising to 21% in cases of prolonged opioid use (>1 month). Risk factors included female gender, age ≥50 years, and step III opioid use.
Despite its impact, OIC was undertreated, with only 42.8% of affected individuals using laxatives, and satisfaction with treatment was moderate (mean score: 7.2/10). The findings highlight the need for improved OIC management, as detailed in “Opioid-Induced Constipation: A Persistent and Undertreated Burden.”
- Dizziness: A feeling of lightheadedness or vertigo. Percocet, like many opioids, cause a drop in blood pressure, creating dizziness, especially when standing up quickly.
- Headache: A common side effect for some users, which is exacerbated by the dehydrating effects of opioids.
Headaches are a consequence of oxycodone’s impact on blood flow or its interaction with other substances in the body.
What Are the Serious Side Effects of Taking Percocet?
Serious side effects of taking Percocet are respiratory depression, liver failure, overdose, addiction and dependence, and hypotension. The FDA issues a black box warning on opioids, emphasizing severe risks such as fatal respiratory failure.
Between 50% and 80% of patients in clinical trials experience at least one side effect from opioid therapy. The incidence is even higher in everyday use, as provided by the Faculty of Pain Medicine of the Royal College of Anaesthetists.
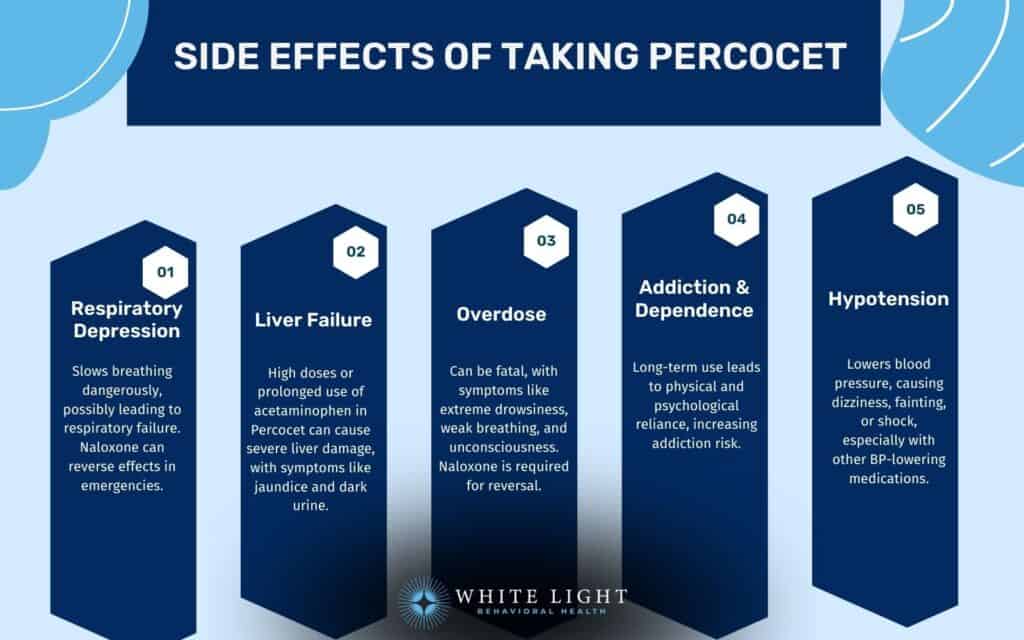
The serious side effects of taking Percocet include:
- Respiratory depression: This ensues when Percocet slows down breathing to dangerous levels, potentially instigating respiratory failure, a life-threatening condition. Symptoms are slow, shallow breathing, extreme drowsiness, and confusion.
If these symptoms appear, immediate medical attention is necessary, and naloxone (an opioid antagonist) is administered to reverse the effects.
- Liver failure: Percocet contains acetaminophen, which engenders liver damage, especially with prolonged use or higher doses. Symptoms are jaundice (yellowing of the skin or eyes), dark urine, and severe abdominal pain.
Liver failure is a life-threatening condition that elicits urgent medical treatment.
Experts agree that taking a large amount of acetaminophen in a short period breeds liver injury. However, a specific threshold for toxicity has not been established and is different between individuals.
Based on current data, they are unable to pinpoint all the factors that shoot up the peril of acetaminophen toxicity, especially at doses close to the recommended maximum daily limit of 4,000 mg, as cited by Regulations.gov.
- Overdose: Overdosing on Percocet has fatal consequences. Symptoms of overdose are extreme drowsiness, slow or difficult breathing, limp muscles, and loss of consciousness.
In the event of an overdose, seek immediate medical help. Naloxone is used to reverse opioid overdose effects, but timely intervention is a prerequisite.
- Addiction and dependence: Extended use of Percocet brings about physical and psychological dependence, making it difficult for individuals to stop using it.
The possibility for addiction rises due to the opioid component, oxycodone. The risk of addiction is a serious concern outlined in opioid safety guidelines.
- Hypotension: Percocet induces a drop in blood pressure, evoking dizziness, fainting, or even shock in severe cases.
This is especially severe when combined with other medications that lower blood pressure.
Can Percocet Affect Your Mental Health?
Yes, Percocet can affect your mental health. Long-term use of Percocet, particularly ascribed to its opioid component oxycodone, hatching mood changes, anxiety, and depression. Opioids have been shown to impact brain chemistry, potentially altering the balance of neurotransmitters that regulate mood and emotional well-being.
Opioid-induced depression suggests that extended opioid use expands the risk of depressive symptoms. This effect is seen in individuals who use opioids over long periods, as the body becomes dependent on the substance, generating mental health challenges.
Santo Jr. et al. 2022 conducted a systematic review and meta-analysis to estimate the prevalence of mental disorders among individuals with opioid use disorder (OUD).
Analyzing data from 345 studies involving 104,135 individuals, they found high rates of comorbid conditions: depression (36.1%), anxiety (29.1%), PTSD (18.1%), ADHD (20.9%), and bipolar disorder (8.7%). Personality disorders were also prevalent, with antisocial personality disorder at 33.6% and borderline personality disorder at 18.2%.
Mental health conditions were more common among women and varied by sample characteristics. These findings highlight the critical need for integrated mental health care in OUD treatment, as discussed in “Mental Health Disorders in Opioid Use Disorder: A Call for Integrated Care.”
What Are the Risks of Misusing Percocet?
The risks of misusing Percocet are addiction, overdose, and mixing with other substances.

Misuse of Percocet has far-reaching ramifications, including:
- Addiction: Recursive misuse of Percocet elicits prescription drug abuse, where individuals develop a dependence on the drug, making it challenging to stop using it despite its negative effects.
- Overdose: Taking too much Percocet amplifies the risk of overdose, which is mostly fatal. Symptoms of an overdose are slow or shallow breathing, extreme drowsiness, and loss of consciousness.
Overdose requires immediate medical intervention, such as the administration of naloxone, an opioid antagonist.
- Mixing with other substances: Combining Percocet with other substances, such as alcohol or benzodiazepines, produces fatal interactions. These combinations substantially depress the central nervous system, spawning respiratory failure or even death.
More than 20% of opioid overdoses involve synthetic opioids, chiefly fentanyl, which is mixed with other substances, causing fatal outcomes, as mentioned by the University of Washington’s Addictions, Drug & Alcohol Institute (ADAI).
Can Percocet Lead to Dependence and Addiction?
Yes, Percocet can lead to dependence and addiction. As an opioid, Percocet binds to opioid receptors in the brain, producing pain relief and feelings of euphoria. Over time, the body builds tolerance, meaning higher doses are needed to achieve the same effect.
This initiates physical dependence, where the body requires the drug to function normally. Continued use brings addiction, where individuals compulsively seek out the drug despite negative consequences.
In the U.S., opioid use disorders, covering Percocet addiction, are a growing concern, with about 5.7 million people in the United States having opioid use disorder in 2023.
Rediscover Life at White Light Behavioral Health
Get the compassionate support you deserve. We're here to help you reclaim joy, wellness, and a brighter future.
Our Facility
How to Take Percocet Safely?
To take Percocet safely, follow your doctor’s prescribed dosage, avoid alcohol and other sedatives, store Percocet securely, monitor for signs of tolerance or dependence, and consult your healthcare provider regularly. By adhering to these doctor-approved guidelines, you cut the risk of detrimental side effects or prescription drug abuse while using Percocet.
The following are ways you take Percocet safely:
- Follow your doctor’s prescribed dosage: Always take Percocet exactly as prescribed by your healthcare provider. Never exceed the recommended dose, and avoid taking it more frequently than directed.
- Avoid alcohol and other sedatives: Do not consume alcohol or use other sedatives (like benzodiazepines) while taking Percocet.
Combining these substances increases the risk of severe side effects, such as respiratory depression or overdose.
- Store Percocet safely: Keep Percocet in a secure place, away from children or anyone that will misuse it. Avoid sharing your medication with others, as it is intended only for your use.
- Monitor for signs of dependence: Be aware of any signs of tolerance or dependence, such as needing higher doses for the same effect or experiencing withdrawal symptoms when not taking the medication.
- Consult your doctor regularly: Schedule follow-up appointments with your healthcare provider to discuss the effectiveness and risks of your treatment.
This allows for adjustments if necessary and helps prevent misuse.
What Should You Avoid While Taking Percocet?
You should avoid alcohol, sedatives, driving, and excessive doses of acetaminophen while taking Percocet. A driver pulled over for suspected impairment while on prescription drugs is arrested for OVI/DUI under Ohio Rev.
Code 4511.19. There are two ways a driver is apprehended for operating a vehicle under the influence of prescription drugs (OVID) in Central Ohio: by being “under the influence” or by having a drug concentration in their urine or blood that exceeds legal limits, as outlined in Ohio Revised Code 4511.19.
According to the National Highway Traffic Safety Administration (NHTSA), 56% of drivers involved in serious injury or fatal crashes who tested positive for at least one drug were reported by trauma centers from October to December 2020.
Here’s a quick list of things to avoid while taking Percocet:
- Alcohol: Combining Percocet with alcohol increases the risk of drowsiness, impaired thinking, and overdose risk. Both substances are CNS depressants, which dangerously degrade your breathing and heart rate.
- Sedatives and tranquilizers: Avoid using other sedatives or tranquilizers with Percocet, as they amplify the CNS depressant effects, leading to extreme drowsiness, respiratory failure, or even death.
- Driving or operating heavy machinery: Percocet causes impaired thinking and drowsiness, making it unsafe to drive or perform tasks requiring full mental alertness.
Operating a vehicle under the influence of Percocet results in DUI charges, depending on state laws.
- Excessive doses of acetaminophen: Taking too much Percocet or using it with other medications containing acetaminophen lead to liver toxicity, especially if you exceed the daily recommended dose.
Can You Take Percocet with Ibuprofen?
Yes, you can take Percocet with ibuprofen under the guidance of a healthcare provider. Combining Percocet, which contains oxycodone, with NSAIDs like ibuprofen is safe for short-term use when prescribed by a doctor, as they work in different ways to manage pain.
It is important to follow dosage instructions closely to avoid potential risks, such as liver damage or increased side effects. Always consult with a healthcare provider before combining medications.
Is Percocet Safe for Long-Term Use?
Long-term use of Percocet is generally not recommended due to the high risk of dependence, tolerance, and probable liver damage. Chronic use of opioids leads to opioid dependence and withdrawal symptoms when the medication is dropped or stopped.
Up to 21% of individuals who use opioids long-term have opioid use disorder. Alternative treatments for managing chronic pain, such as physical therapy or non-opioid medications, are indicated to lessen these risks.
The American Medical Association (AMA) estimates that between 3% and 19% of individuals who use prescription pain medications develop an addiction.
How Long Does Percocet Stay in Your System?
Percocet stays in your system in the blood for 24 hours, urine for up to 4 days, and saliva for 2 days, with hair tests showing traces for up to 90 days.
What Are the Safer Alternatives to Percocet?
The safer alternatives to Percocet include NSAIDs, acetaminophen, physical therapy, Cognitive Behavioral Therapy (CBT), nerve blocks and injections, acupuncture, and cold and heat therapy. For example, in the United States, the National Health Interview Survey reveals that acupuncture use among adults more than doubled from 2002 to 2022, rising from 1.0% in 2002 to 2.2% in 2022.
The safer alternatives to Percocet are given below:
- NSAIDs (Non-Steroidal Anti-Inflammatory Drugs): Medications like ibuprofen and naproxen reduce inflammation and pain without opioid-related risks. Studies have shown their effectiveness in managing musculoskeletal pain.
- Acetaminophen: A frequently used pain reliever effective for mild to moderate pain but must be taken within safe dosage limits to prevent liver toxicity.
It is used in combination with other treatments for enhanced pain relief.
- Physical Therapy: Structured exercises and manual therapy techniques that improve mobility and decrease pain by addressing the root cause rather than masking symptoms. It offers long-term benefits for managing chronic pain conditions.
- Cognitive Behavioral Therapy (CBT): A psychological approach that helps manage chronic pain by altering pain perception and coping mechanisms.
Research supports its role in reducing reliance on medications. Cognitive Behavioral Therapy (CBT) has an effectiveness rate of 50-75%, majorly trimming substance use and supporting long-term recovery, making it a key component in addiction treatment programs, as explored by Pybis, Jo, et al. 2017 in “The Comparative Effectiveness and Efficiency of Cognitive Behaviour Therapy and Generic Counselling in the Treatment of Depression: Evidence from the 2nd UK National Audit of Psychological Therapies.”
- Nerve Blocks and Injections: Local anesthetics and corticosteroid injections provide targeted pain relief, reducing the need for systemic medications.
They are particularly effective for addressing neuropathic and inflammatory pain.
- Acupuncture: A holistic treatment that stimulates nerves and muscles to alleviate pain through natural pain-relief mechanisms.
Vickers et al. 2012 conducted an individual patient data meta-analysis to evaluate acupuncture’s effectiveness for chronic pain. Analyzing 29 randomized controlled trials with 17,922 patients, they found acupuncture reduced pain compared to both sham and no-acupuncture controls.
Pain relief of 50% or more on a 100-point scale – pain that drops from a 60 to a 30, say – is utilized as a standard of effectiveness in pain research. By this measure, the study found, the effectiveness rates for real acupuncture, sham acupuncture, and treatment, as usual, are 50%, 43%, and 30%, respectively, as elaborated in “Acupuncture for Chronic Pain: Modest but Real Benefits.”
- Cold and Heat Therapy: The use of ice packs reduces swelling and inflammation, while heat therapy relaxes muscles and ameliorates circulation to ease discomfort. These methods are productive for acute injuries and chronic pain relief.
Are you covered for treatment?
White Light Behavioral Health is an approved provider for Blue Cross Blue Shield and TUFTS, while also accepting many other major insurance carriers.
Check Coverage Now!Is Morphine Stronger than Percocet?
Morphine is stronger than Percocet. Morphine is a pure opioid analgesic, whereas Percocet contains oxycodone and acetaminophen, making it less potent for severe pain.
Fassassi et al. 2021 conducted a randomized, double-blind trial to compare the analgesic efficacy of Morphine Sulfate Immediate Release (MSIR) with Acetaminophen versus Oxycodone/Acetaminophen (Percocet) for acute pain in the emergency department (ED). The study included 80 patients with moderate to severe pain (NRS ≥5), who received either 15 mg MSIR + 650 mg Acetaminophen or 10 mg Oxycodone + 650 mg Acetaminophen.
Pain scores declined similarly in both groups over 60 minutes, with a mean reduction of 4.2 (MSIR, 49.8%) versus 3.61 (Percocet, 42.3%).
Both treatments were effective, with no serious adverse events, but MSIR had lower drug likeability, suggesting it is a viable opioid alternative, as indicated in “Analgesic Efficacy of Morphine Sulfate Immediate Release vs. Oxycodone/Acetaminophen for Acute Pain in the Emergency Department.” The trial doesn’t necessarily contradict the general understanding that morphine is more potent than Percocet on an equianalgesic basis—potency is highly dependent on dosing, formulation, and clinical context.
Is Percocet Stronger than Hydrocodone?
No, Percocet is not stronger than hydrocodone. According to Slawson D. in “No Difference Between Oxycodone/Acetaminophen and Hydrocodone/Acetaminophen for Acute Extremity Pain,” a randomized trial comparing the two found no major difference in pain reduction for acute musculoskeletal extremity pain.
In the study, which included diagnoses such as approximately 65% fractures, 40% sprains and strains, and 5% other conditions, intention-to-treat analyses revealed similar mean pain score reductions between the oxycodone/acetaminophen group (Percocet) and the hydrocodone/acetaminophen group, with roughly 60% of patients in each group reporting at least a 50% decrease in pain. Hydrocodone, a semi-synthetic opioid used for moderate to severe pain, demonstrates comparable analgesic efficacy to Percocet in this clinical context.
Share This Post
















