Naltrexone: How It Helps, Safe Use, and Comparable Medications

Looking for help overcoming alcohol or opioid addiction, then Naltrexone is the answer. Naltrexone is an opioid antagonist that treats opioid use disorder and alcohol dependence by blocking cravings and effects. It works by blocking the receptors in your brain that cause those intense cravings and euphoric feelings from drinking or using.
According to the Ohio Board of Pharmacy’s 2020 Annual Report, 4,745 prescribers issued naltrexone prescriptions to 25,514 patients in 2020.
Naltrexone treats opioid and alcohol use disorders by reducing cravings and preventing relapse, as a 50 mg daily oral tablet or a 380 mg monthly intramuscular injection. Side effects include nausea or headaches, but higher doses may cause more serious reactions.
Alternatives to Naltrexone for addiction include Buprenorphine, Methadone, Acamprosate, Disulfiram, Topiramate, and Gabapentin. You should avoid naltrexone if you are currently using opioids, have severe liver disease, are pregnant or breastfeeding, or have severe kidney disease.
What Is Naltrexone?
Naltrexone is an opioid antagonist medication used to treat opioid use disorder and alcohol dependence. It works by blocking the effects of opioids in the brain, preventing euphoria and reducing cravings.
Unlike opioids, Naltrexone is non-addictive and does not cause physical dependence. Common brand names include Vivitrol and ReVia. As part of medication-assisted treatment (MAT), Naltrexone helps you manage addiction by reducing the risk of relapse.
Did you know most health insurance plans cover substance use disorder treatment? Check your coverage online now.
What Is the Mechanism of Action of Naltrexone?
Naltrexone works by blocking opioid receptors in the brain, specifically the mu-opioid receptors, which are responsible for the euphoric and sedative effects that make opioids and alcohol so addictive. By preventing these receptors from being activated, Naltrexone eliminates the pleasure associated with alcohol or opioid use, making it easier to stay sober.
Naltrexone helps with alcohol dependence by regulating neurotransmitter activity, particularly reducing the excessive dopamine release that drives cravings. This makes it easier to manage urges and stay on track with recovery.
The oral form of Naltrexone has a bioavailability of 5 to 40%, meaning it’s absorbed into the bloodstream at varying levels. It stays active for about 24 hours. The injectable version, on the other hand, offers longer-lasting effects, blocking receptors for several weeks, which is especially helpful for those who prefer less frequent dosing.
How Is Naltrexone Used in Addiction Treatment?
Naltrexone is used in addiction treatment to support individuals recovering from opioid and alcohol use disorders by reducing cravings and preventing relapse. In opioid addiction, it blocks the effects of opioids, discouraging their use.
More Resources on Addiction:
In alcohol use disorder, it decreases the rewarding effects of alcohol, helping individuals reduce consumption. As a key component of medication-assisted treatment, it is combined with therapy and support programs for long-term recovery.
How Is Naltrexone Taken?
Naltrexone is taken as a daily oral tablet or as a long-acting monthly injection, depending on the individual’s treatment plan and medical needs. Both forms help support addiction recovery by reducing cravings and preventing relapse.
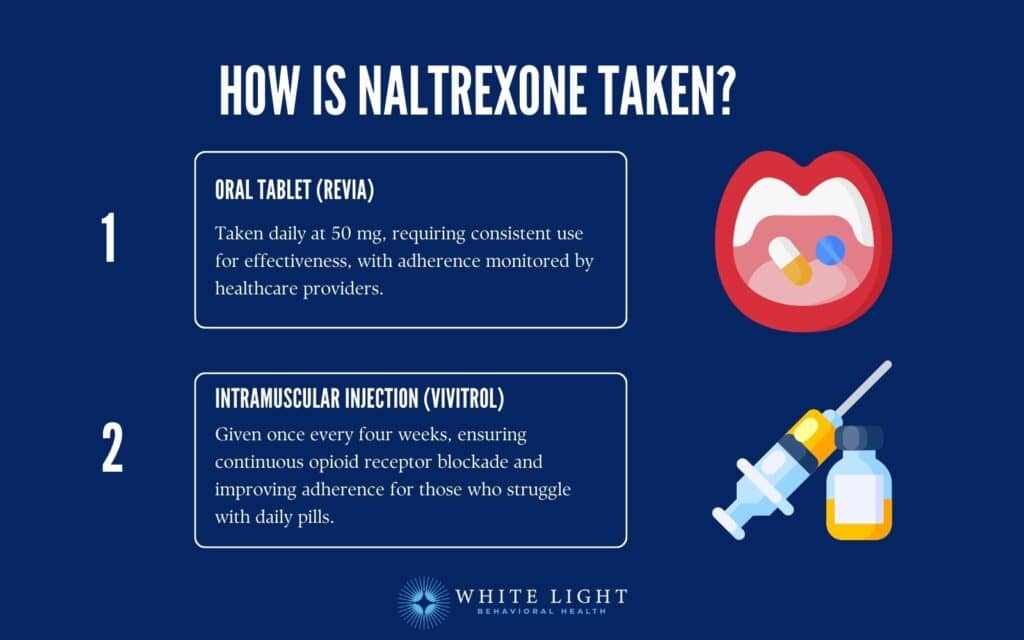
Ways naltrexone is taken include:
- Oral Tablet (ReVia): The oral form is prescribed at a dose of 50 mg per day. It must be taken consistently to maintain opioid and alcohol blockade.
Because adherence is required for effectiveness, healthcare providers monitor patients to ensure regular use.
- Intramuscular Injection (Vivitrol): This extended-release injection is administered by a healthcare professional once every four weeks. It provides continuous opioid receptor blockade, eliminating the need for daily dosing and improving adherence for individuals who struggle with taking a daily pill.
What Is the Recommended Dosage for Naltrexone?
The recommended dosage of Naltrexone is 50 mg per day for the oral tablet (ReVia) in the treatment of alcohol dependence and opioid use disorder.
For individuals receiving the extended-release injectable form (Vivitrol), the standard dose is 380 mg administered intramuscularly once every four weeks.
In some cases, dosage adjustments are made based on patient response and tolerability. Lower starting doses, such as 25 mg, are used initially to assess tolerance, particularly for individuals transitioning from opioid use.
Before starting Naltrexone for opioid use disorder, patients must be opioid-free for at least 10 days to avoid precipitated withdrawal.
What Are the Side Effects of Naltrexone?
The side effects of Naltrexone are mild to moderate, with nausea, headache, and injection site reactions being the most commonly reported. While many users tolerate the medication well, some experience more severe reactions that require medical attention.

The side effects of Naltrexone are as follows:
- Common Side Effects: Nausea, headache, dizziness, fatigue, and gastrointestinal discomfort are frequently reported, especially when starting treatment. These effects are mild and resolve as the body adjusts to the medication.
- Moderate Side Effects: Some users experience sleep disturbances, anxiety, muscle pain, or decreased appetite.
While these effects are bothersome, they usually do not require discontinuation of the medication.
- Severe Side Effects: In rare cases, Naltrexone causes liver toxicity, severe allergic reactions, or significant depression. The extended-release injection also leads to serious injection site reactions, including pain, swelling, and tissue damage.
Patients experiencing severe or persistent symptoms should seek medical attention.
Contact us today to schedule an initial assessment or to learn more about our services. Whether you are seeking intensive outpatient care or simply need guidance on your mental health journey, we are here to help.
How Long Do Naltrexone Side Effects Last?
Naltrexone side effects last for a few days to a few weeks, depending on the individual and the medication’s form. Mild side effects, such as nausea and headache, usually subside within a few days to a week as the body adjusts.
Injection site reactions from the extended-release form (Vivitrol) last longer, sometimes persisting for up to two weeks. Severe or persistent side effects should be reported to a healthcare provider.
Can Naltrexone Cause Withdrawal Symptoms?
No, Naltrexone cannot cause withdrawal symptoms on its own, as it is not an opioid and does not create dependence. However, if opioids are still in the system when Naltrexone is taken, it triggers precipitated withdrawal, which is a sudden and severe withdrawal reaction.
Does Low-Dose Naltrexone Cause Liver Damage?
No, low-dose Naltrexone does not cause liver damage and is considered safe. However, individuals with preexisting liver conditions should undergo regular monitoring as a precaution.
How Can You Manage or Reduce the Side Effects of Naltrexone?
You can manage or reduce the side effects of Naltrexone by taking simple precautions such as adjusting the timing of doses, staying hydrated, and consulting your doctor about possible dosage changes.
- Take with Food: Consuming Naltrexone with food helps reduce nausea and gastrointestinal discomfort, which are common initial side effects.
- Stay Hydrated: Drinking plenty of water helps alleviate headaches and dizziness that some users experience when starting treatment.
- Monitor Injection Sites: For those receiving the extended-release injection, applying a cold compress and avoiding excessive pressure on the site helps minimize pain and swelling.
- Adjust Dosage Under Medical Supervision: If side effects persist or worsen, a healthcare provider adjusts the dose or recommends strategies to improve tolerance.
Is Naltrexone Safe for Long-Term Use?
Yes, Naltrexone is safe for long-term use when taken as prescribed. However, regular liver function monitoring is recommended, especially in individuals with preexisting liver conditions.
Rediscover Life at White Light Behavioral Health
Get the compassionate support you deserve. We're here to help you reclaim joy, wellness, and a brighter future.
Our Facility
Can You Stop Taking Naltrexone Suddenly?
Yes, you can stop taking Naltrexone suddenly without experiencing withdrawal symptoms because it does not cause physical dependence. However, discontinuing Naltrexone increases relapse risk, so it is advisable to consult a healthcare provider before stopping treatment to discuss alternative relapse prevention strategies.
What Are the Alternatives to Naltrexone for Addiction?
The alternatives to Naltrexone for addiction are Buprenorphine, Methadone, Acamprosate, Disulfiram, Topiramate, and Gabapentin. These medications work to block the effects of addictive substances as part of medication-assisted treatment (MAT) programs.
The alternatives to naltrexone for addiction include:
Buprenorphine
Buprenorphine is a partial opioid agonist that reduces withdrawal symptoms and cravings without producing a strong high. It is combined with Naloxone (Suboxone) to prevent misuse and is a widely used treatment for opioid use disorder.
Methadone
Methadone is a full opioid agonist that stabilizes brain chemistry by preventing withdrawal symptoms and reducing cravings. It is dispensed in specialized clinics and is highly effective in maintaining long-term recovery from opioid addiction.
Acamprosate (Campral)
Acamprosate is used for alcohol use disorder. It helps restore neurotransmitter balance in the brain, reducing alcohol cravings and preventing relapse. Those who have already stopped drinking can find Acamprosate particularly beneficial in their recovery efforts.
Are you covered for treatment?
White Light Behavioral Health is an approved provider for Blue Cross Blue Shield and TUFTS, while also accepting many other major insurance carriers.
Check Coverage Now!Disulfiram (Antabuse)
Disulfiram is a medication that discourages alcohol consumption by causing unpleasant reactions (such as nausea and flushing) when alcohol is ingested. This approach helps reinforce abstinence in individuals committed to sobriety, making Disulfiram an effective tool in their recovery.
Topiramate
Topiramate is an anticonvulsant medication that has been shown to reduce alcohol cravings and heavy drinking episodes by modulating brain activity. Though not FDA-approved for addiction treatment, it is sometimes used off-label.
Gabapentin
Gabapentin is another anticonvulsant that helps with alcohol withdrawal symptoms and reduces cravings. It is also used off-label for alcohol use disorder, especially in individuals with co-occurring anxiety or insomnia.
How Does Naltrexone Differ from Buprenorphine and Methadone for Opioid Use Disorder?
Naltrexone differs from Buprenorphine and Methadone for opioid use disorder (OUD) in that it is an opioid antagonist, meaning it completely blocks opioid effects without activating opioid receptors. In contrast, Buprenorphine is a partial agonist, and Methadone is a full agonist, both of which reduce cravings and withdrawal by stimulating opioid receptors to varying degrees.
The table below shows how naltrexone differs from buprenorphine and methadone for opioid use disorder:
| Factor | Naltrexone (Vivitrol) | Buprenorphine (Suboxone, Subutex) | Methadone (Dolophine) |
| Mechanism of Action | Opioid antagonist; blocks opioid effects completely | Partial opioid agonist; activates receptors mildly to reduce cravings | Full opioid agonist; activates receptors fully to prevent withdrawal |
| Effectiveness | Most effective for relapse prevention in opioid-free individuals | Reduces cravings and withdrawal, effective for maintenance treatment | Highly effective for severe OUD and long-term stabilization |
| Dependence Risk | Non-addictive, does not cause dependence | Low risk of dependence; has a ceiling effect to limit misuse | Higher risk of dependence; long-term use requires tapering |
| Best For | Individuals who are fully detoxed and want to prevent relapse | Those needing both craving and withdrawal management | Individuals with severe addiction needing structured, long-term support |
While all three medications are used in medication-assisted treatment (MAT) to treat opioid use disorder, the main difference lies in their mechanism of action and dependence risk.
Who Should Avoid Taking Naltrexone?
Individuals with current opioid use, severe liver disease, or certain medical conditions should avoid taking Naltrexone, as it causes precipitated withdrawal or worsens underlying health issues. According to FDA guidelines, Naltrexone is contraindicated in patients who have not fully detoxed from opioids or have significant liver impairment.
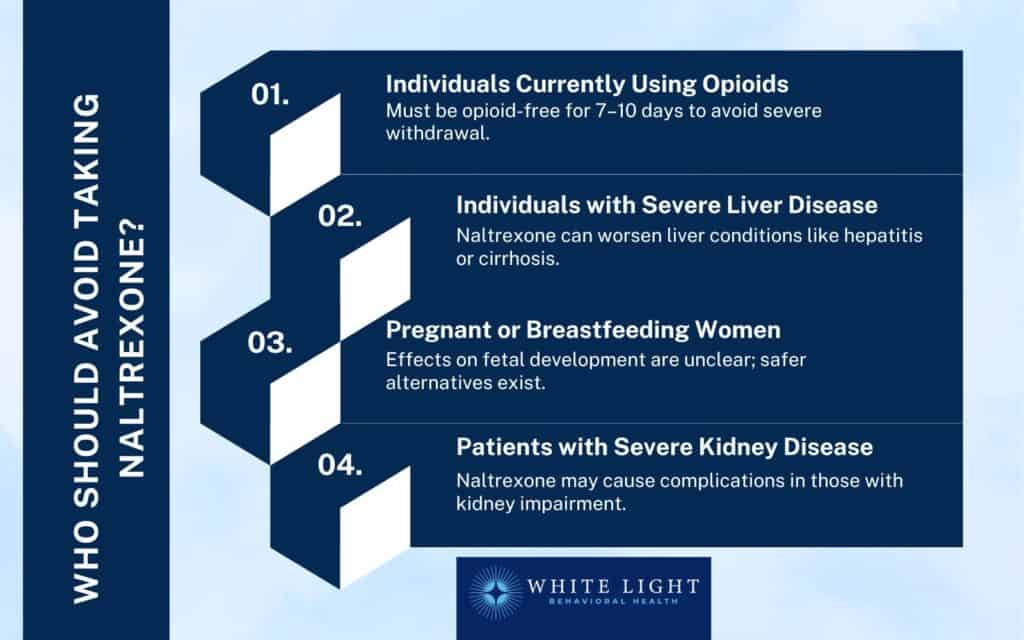
- Individuals Currently Using Opioids: Naltrexone is an opioid antagonist, meaning it blocks opioid effects. Taking it while opioids are still in the system triggers precipitated withdrawal, a sudden and severe withdrawal reaction.
Patients must be opioid-free for at least 7 to 10 days before starting Naltrexone.
- Individuals with Severe Liver Disease: Naltrexone is processed by the liver, and high doses have been linked to hepatotoxicity (liver toxicity). Patients with conditions like hepatitis or cirrhosis should use caution or avoid it entirely, as it worsens liver function.
- Pregnant or Breastfeeding Women: While research on Naltrexone use during pregnancy is limited, the FDA advises caution, as its effects on fetal development are not fully understood.
Buprenorphine or Methadone are recommended alternatives for pregnant individuals with opioid use disorder.
- Patients with Severe Kidney Disease: Though rare, Naltrexone causes complications in patients with renal impairment, as it is partially excreted by the kidneys. Healthcare providers consider alternative treatments in these cases.
What Happens if You Take Tramadol and Naltrexone Together?
If you take Tramadol and Naltrexone together, Naltrexone will block the opioid effects of Tramadol, reducing its pain-relieving properties and making it ineffective. Taking Naltrexone while Tramadol is in their system triggers withdrawal symptoms due to opioid blockade if a person is opioid-dependent.
Did you know most health insurance plans cover substance use disorder treatment? Check your coverage online now.
Can You Drink Alcohol While on Naltrexone?
Yes, you can drink alcohol while on Naltrexone because it does not cause sickness like Disulfiram (Antabuse). However, Naltrexone reduces the pleasurable effects of alcohol by blocking opioid receptors, which helps decrease cravings and make drinking less appealing. It is commonly used in medication-assisted treatment (MAT) for alcohol use disorder to support long-term recovery.
How to Get Naltrexone in Columbus, Ohio?
To get Naltrexone in Columbus, Ohio, you need a prescription from a licensed healthcare provider. It is available through primary care physicians, addiction treatment clinics, telemedicine services, and medication-assisted treatment (MAT) programs.
The oral tablet (ReVia) is filled at most pharmacies, while the extended-release injection (Vivitrol) is administered in a clinic or healthcare setting.
The Ohio Board of Pharmacy’s 2020 Annual Report notes that naltrexone prescriptions are reported to the Ohio Automated Rx Reporting System (OARRS) only when dispensed by pharmacies, excluding those personally furnished by prescribers.
Do You Need a Prescription for Naltrexone in Columbus, Ohio?
Yes, you need a doctor’s prescription for Naltrexone in Columbus, Ohio. Because it is a controlled medication used for opioid and alcohol dependence treatment, it must be prescribed and monitored by a healthcare provider to ensure safe and effective use.
Is Naltrexone Covered by Insurance in Ohio?
Yes, naltrexone is covered by insurance in Ohio, but coverage varies depending on the provider and policy. The oral tablet version is more affordable, while the injectable form (Vivitrol) is costly without insurance, with out-of-pocket costs ranging from $800 to $1,500 per month. Patients should check with their insurance provider for specific coverage details.
How Long Does Naltrexone Stay in Your System?
Naltrexone stays in your system for 24 to 48 hours after an oral dose, with a half-life of 4 to 6 hours. The injectable (Vivitrol) form lasts much longer, staying in the body for 5 to 10 days. In drug tests, Naltrexone is not screened for, but if tested, it is detectable in urine for up to 24 hours, blood for a few days, saliva for a short period, and hair for up to 90 days.
Share This Post
















