Alcohol Addiction Programs: Definition, Types, Treatments, Cost

Alcohol addiction programs are structured treatment plans designed to help individuals overcome alcohol dependence and achieve long-term sobriety. These programs incorporate medical, psychological, and behavioral interventions to address the physical and mental health challenges associated with alcohol use disorder (AUD). They provide a supportive environment where individuals develop coping strategies, rebuild their lives, and prevent relapse.
The main types of alcohol addiction programs include inpatient, outpatient, detox, and 12-step programs, each catering to different levels of addiction severity and personal needs. Inpatient rehab offers 24/7 medical supervision and an immersive recovery environment, while outpatient programs allow individuals to receive treatment while maintaining daily responsibilities.
Detox programs help manage withdrawal symptoms safely, and support groups like Alcoholics Anonymous (AA) provide peer-based recovery support. Choosing the right program depends on factors like addiction severity, medical history, and personal circumstances.
Treatment options in alcohol addiction programs are diverse and evidence-based. Medication-assisted treatment (MAT) includes FDA-approved medications like naltrexone, acamprosate, and disulfiram to reduce cravings and prevent relapse.
Behavioral therapies, such as Cognitive-Behavioral Therapy (CBT) and Motivational Enhancement Therapy (MET), help individuals modify harmful drinking behaviors. Counseling, holistic therapies, and aftercare programs further support long-term recovery by addressing emotional and social challenges.
The cost of alcohol addiction programs varies depending on factors like treatment type, program duration, location, and level of care provided. Inpatient rehab costs $6,000 to $60,000 per month, while outpatient programs range from $1,000 to $10,000 per month.
Many insurance plans cover addiction treatment, but coverage depends on policy details, deductibles, and co-pays. Financial aid, sliding scale fees, and government-funded programs help make treatment more accessible.
What Is an Alcohol Addiction Program?
An alcohol addiction program is a structured treatment plan designed to help individuals overcome alcohol dependence through medical, psychological, and behavioral interventions. These programs, which are inpatient or outpatient, include detoxification, counseling, medication-assisted treatment, and relapse prevention strategies.
More Resources on Addiction:
According to the 2023 National Survey on Drug Use and Health (NSDUH), 2.3 million people ages 12 and older who had alcohol use disorder (AUD) in the past year (7.9% of people with past-year AUD in this age group) received alcohol use treatment in the past year.
Research from the National Institute on Alcohol Abuse and Alcoholism (NIAAA) highlights that comprehensive treatment programs significantly improve recovery outcomes, with structured programs increasing abstinence rates by 40 to 60%. Such programs are important as untreated alcohol addiction contributes to over 3 million deaths globally each year, according to the World Health Organization (WHO).
Did you know most health insurance plans cover substance use disorder treatment? Check your coverage online now.
How Do Alcohol Addiction Programs Work?
Alcohol addiction programs work by addressing both the physical and psychological aspects of addiction through a combination of detox, therapy, and support systems. These programs begin with medical detoxification to manage withdrawal symptoms, followed by behavioral therapies like Cognitive Behavioral Therapy (CBT) and group counseling to modify drinking behaviors.
According to the Substance Abuse and Mental Health Services Administration (SAMHSA), medication-assisted treatments like naltrexone and acamprosate further enhance recovery rates by reducing cravings and relapse risks. Long-term success is reinforced through aftercare planning, peer support groups, and relapse prevention strategies, ensuring sustained sobriety.
What Are the Different Types of Alcohol Addiction Programs?
The different types of alcohol addiction programs include inpatient rehab, outpatient programs, detox programs, and 12-step programs, each catering to different levels of alcohol dependence and recovery needs. These programs are designed to provide medical, psychological, and peer support while complying with healthcare regulations and addiction treatment best practices.

The different types of alcohol addiction programs are as follows:
1. Inpatient Rehab
Inpatient rehab programs require individuals to stay at a treatment facility for a structured and intensive recovery process, typically lasting 30 to 90 days.
These programs provide 24/7 medical supervision, evidence-based therapies, and medication-assisted treatment (MAT) to manage withdrawal and prevent relapse. Legally, inpatient rehab centers must comply with the Substance Abuse and Mental Health Services Administration (SAMHSA) guidelines and licensing requirements set by state health departments.
Studies indicate that inpatient rehab significantly improves long-term recovery outcomes, with a reported 50-60% reduction in relapse rates.
2. Outpatient Programs
Outpatient programs allow individuals to receive treatment while continuing their daily responsibilities, offering flexibility for work and family commitments.
These programs include counseling, behavioral therapy, and support group meetings, meeting state and federal treatment standards. According to the National Institute on Alcohol Abuse and Alcoholism (NIAAA), outpatient treatment is effective for mild-to-moderate alcohol use disorder, with success rates comparable to inpatient care when combined with strong social support.
Intensive outpatient programs (IOPs) and partial hospitalization programs (PHPs) provide structured care without requiring overnight stays. According to the National Association for Behavioral Health, in 2022, there were approximately 1,380-day treatment programs, also known as Partial Hospitalization Programs (PHPs), across the U.S., designed for individuals with mental illness or co-occurring disorders. IOPs show high-quality evidence indicating that IOPs produce outcomes comparable to inpatient care, with significant reductions in alcohol and drug use, though variations exist in program structures and outcome measurements, as studied by McCarty D et al. 2014, titled “Substance abuse intensive outpatient programs: assessing the evidence.”
Research by Miller CB et al. 2020 titled “Feasibility and efficacy of a digital CBT intervention for symptoms of Generalized Anxiety Disorder: A randomized multiple-baseline study” indicates that CBT combined with other therapies leads to a 60% reduction in relapse rates. Similarly, a study by Maffei C et al. 2018, titled “Dialectical Behavior Therapy Skills Training in Alcohol Dependence Treatment: Findings Based on an Open Trial,” involving 244 subjects found that 73.2% of the 157 patients who completed a Dialectical Behavior Therapy Skills Training (DBT-ST) program were abstinent at the program’s end.
3. Detox Programs
Detox programs focus on safely managing alcohol withdrawal symptoms through medical supervision, serving as the first step in recovery.
Medically-assisted detox is important for individuals with severe alcohol dependence, as withdrawal leads to life-threatening complications like seizures and delirium tremens (DTs). Facilities offering detox must adhere to healthcare regulations and medical best practices, including protocols established by the American Society of Addiction Medicine (ASAM).
According to SAMHSA, 68% of people who complete drug and alcohol detox programs report their treatment to be successful. The medically supervised detox programs reduce withdrawal-related fatalities and improve transition into long-term treatment.
The success rate of detoxification is higher when combined with ongoing therapy and support, with Bailey GL, Herman DS, Stein MD. et al. 2013, in their study titled “Perceived relapse risk and desire for medication-assisted treatment among persons seeking inpatient opiate detoxification,” shows that 70- to 80% of individuals who undergo detox successfully start their recovery journey with reduced risk of relapse.
Contact us today to schedule an initial assessment or to learn more about our services. Whether you are seeking intensive outpatient care or simply need guidance on your mental health journey, we are here to help.
4. 12-Step Programs
12-step programs, such as Alcoholics Anonymous (AA), follow a peer-support model centered on spiritual and personal growth.
These programs emphasize accountability, community support, and structured recovery steps to help individuals achieve long-term sobriety. While not a replacement for medical treatment, 12-step programs are legally recognized as mutual aid groups and are incorporated into professional addiction treatment plans.
A study by Friedman, R. 2014, titled “Taking Aim at 12-Step Programs,” has shown that participation in AA significantly increases the likelihood of long-term sobriety up to 66% by providing a supportive community and emotional connection.
5. Holistic and Alternative Treatment Programs
Holistic alcohol addiction programs incorporate non-traditional therapies such as yoga, meditation, acupuncture, and nutritional counseling to address the mental, emotional, and physical aspects of addiction. These programs operate under wellness-focused regulations and complement evidence-based treatments.
Research by Wild B. et al. 2020, titled “Acupuncture in Persons with an Increased Stress Level-Results from a Randomized-controlled Pilot Trial,” suggests acupuncture significantly reduces stress levels. Acupuncture enhances relaxation, while a National Center for Complementary and Integrative Health study shows that yoga reduces cravings and improves mood during recovery.
6. Medication-Assisted Treatment (MAT) Programs
MAT programs use FDA-approved medications like naltrexone, acamprosate, and disulfiram to reduce alcohol cravings and prevent relapse.
These programs are regulated by the Drug Enforcement Administration (DEA) and SAMHSA, ensuring safe and controlled medication use. According to SAMHSA, MAT increases treatment retention rates by 50% and significantly reduces alcohol relapse rates when combined with counseling and behavioral therapies.
Combining medication with therapy enhances treatment outcomes, according to a study by Anton RF. et al. 2008, titled “Naltrexone for the management of alcohol dependence,” indicating that individuals taking naltrexone combined with therapy are 25% more likely to remain abstinent than those who do not.
What Are the Benefits of Alcohol Addiction Programs?
The benefits of alcohol addiction programs are providing a structured recovery process, ensuring medical safety, and equipping individuals with coping strategies for long-term sobriety. These programs address both the physical and psychological aspects of addiction, significantly improving recovery outcomes and mental well-being.
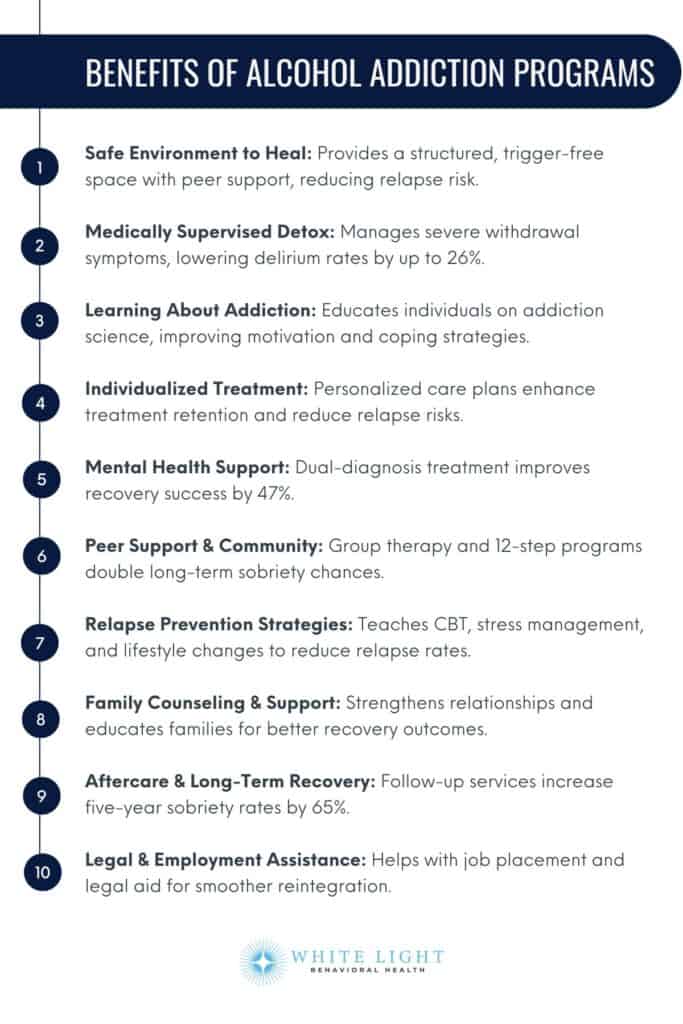
The benefits of alcohol addiction programs are as follows:
1. A Safe Environment to Heal: Alcohol addiction programs provide a controlled and supportive setting where individuals focus entirely on their recovery.
These facilities eliminate external triggers and access to alcohol, reducing the risk of relapse. Structured environments improve recovery success rates by fostering accountability and peer support.
2. Medically Supervised Detox: Detoxing from alcohol leads to severe withdrawal symptoms, including seizures and delirium tremens (DTs), which require medical intervention.
Medically supervised detox ensures that individuals receive professional care, including medication-assisted treatment (MAT) to ease withdrawal discomfort. Medically supervised detox reduces the incidence of delirium, with a study by Kostas TR, Zimmerman KM, Rudolph JL. et al. 2013, titled “Improving delirium care: prevention, monitoring, and assessment,” showing detox lowers delirium rates by up to 26%.
3. Learning About Addiction: Understanding the science behind alcohol addiction helps individuals recognize triggers and develop coping strategies.
Educational programs within rehab facilities teach patients about the neurological and behavioral aspects of addiction, empowering them to make informed decisions about their recovery. A study by Yeh MY, Tung TH, Horng FF, Sung SC. et al. 2017, titled “Effectiveness of a psychoeducational program in enhancing motivation to change alcohol-addictive behavior,” found that after the psychoeducational program, the experimental group showed significantly higher motivation for a change compared to the control group, with measurable increases in recognition and ambivalence
4. Individualized Treatment Programs: Every individual experiences addiction differently, making personalized treatment necessary for effective recovery.
Alcohol addiction programs assess personal history, mental health conditions, and severity of addiction to create customized treatment plans. According to the National Institute on Drug Abuse (NIDA), individualized care improves treatment retention and reduces relapse risks.
5. Mental Health Support: Many individuals struggling with alcohol addiction also suffer from co-occurring mental health disorders like depression and anxiety.
Dual-diagnosis treatment in rehab programs ensures that both addiction and underlying psychiatric conditions are addressed simultaneously. Research by CAMH titled “Mental Illness and Addiction: Facts and Statistics” indicates that individuals with mental health disorders are about twice as likely to develop substance use disorders as those without.
Data suggests that integrated treatment for co-occurring disorders increases recovery success by 47%, according to a study by Wüsthoff LE, Waal H, and Gråwe RW. et al. 2014, titled “The effectiveness of integrated treatment in patients with substance use disorders co-occurring with anxiety and/or depression–a group randomized trial.”
6. Peer Support and Community Connection: Participating in group therapy, 12-step programs, and peer support groups fosters a sense of belonging and shared experiences. Individuals engaged in peer support are twice as likely to maintain long-term sobriety compared to those who attempt recovery alone.
7. Relapse Prevention Strategies: Alcohol addiction programs teach necessary relapse prevention techniques, including cognitive-behavioral therapy (CBT), stress management, support groups, and lifestyle changes.
According to a survey of members of AA, 75% experience a relapse during their first year of recovery. For those who are sober 5 years, the rate drops to 7%.
8. Family Counseling and Support: Addiction affects the individual and their loved ones.
Family therapy in rehab programs helps rebuild trust, improve communication, and educate family members on how to support their loved one’s recovery. Family involvement in treatment leads to better recovery outcomes.
9. Aftercare and Long-Term Recovery Planning: Sustained recovery requires ongoing support, and alcohol addiction programs provide aftercare services such as outpatient therapy, sober living arrangements, and follow-up counseling. Data from SAMHSA shows that individuals who engage in aftercare programs have a 65% higher chance of maintaining sobriety for five years or more.
10. Legal and Employment Assistance: Many rehab programs offer legal aid and vocational training to help individuals reintegrate into society. These services assist with expunging addiction-related charges, finding employment, and rebuilding financial stability, which are necessary for long-term recovery success.
What Are the Challenges of Alcohol Addiction Programs?
The challenges of alcohol addiction programs include relapse risk, cost and accessibility, and commitment and motivation. Despite their effectiveness, these programs face several obstacles impacting recovery outcomes. Understanding these challenges is important for improving treatment strategies and long-term sobriety success.

The challenges of alcohol addiction programs are as follows:
1. Relapse Risk: Relapse remains one of the biggest challenges in alcohol addiction programs, with relapse rates during early recovery are high, with up to 40% to 60% of individuals experiencing relapse in the first year of recovery, according to a study by the National Institute on Drug Abuse (NIDA) et al. 2020, titled “How effective is drug addiction treatment?” This risk is influenced by biological, psychological, and social factors, including cravings, stress, and lack of support. Medically supervised programs address relapse prevention through behavioral therapy, medication-assisted treatment (MAT), and long-term aftercare strategies.
2. Cost and Accessibility: The cost of alcohol addiction treatment varies significantly, with inpatient rehab programs ranging from $6,000 to $20,000 per month, making them financially challenging for many individuals.
Limited insurance coverage and regional disparities in treatment availability further hinder access. Government regulations, such as the Mental Health Parity and Addiction Equity Act (MHPAEA), aim to ensure fair insurance coverage, but gaps in affordability and accessibility persist.
3. Commitment and Motivation: Sustained recovery requires strong personal commitment and motivation, which is difficult due to denial, mental health conditions, or external pressures.
Many individuals struggle with staying engaged in treatment, leading to dropouts. Motivational enhancement therapy (MET) and contingency management (CM) are evidence-based approaches used to improve engagement and adherence in alcohol addiction programs.
4. Co-Occurring Mental Health Disorders: Many individuals with alcohol addiction also suffer from co-occurring mental health conditions such as depression, anxiety, or PTSD. About 37% of people who misuse alcohol or have an alcohol dependence also have at least one serious mental health disorder, according to Alcohol.org.
This dual diagnosis complicates treatment, requiring an integrated approach that combines addiction therapy with psychiatric care. Regulatory guidelines emphasize the need for dual-diagnosis treatment programs, but many facilities lack adequate mental health resources.
5. Stigma and Social Barriers: The stigma associated with alcohol addiction discourages individuals from seeking help and fearing judgment from society, employers, or even family members.
This stigma prevents early intervention and leads to worsening addiction. Legal protections, such as the Americans with Disabilities Act (ADA), prohibit discrimination based on substance use disorders, but societal perceptions still pose a significant barrier.
6. Limited Long-Term Support: Many alcohol addiction programs focus on short-term treatment but lack sufficient long-term support mechanisms.
Ongoing aftercare, including support groups and therapy, significantly reduces relapse rates. However, not all programs provide structured post-treatment support, making sustained recovery more challenging.
Rediscover Life at White Light Behavioral Health
Get the compassionate support you deserve. We're here to help you reclaim joy, wellness, and a brighter future.
Our Facility
What Are the Risks of Quitting Alcohol without a Program?
The risks of quitting alcohol addiction programs include Alcohol Withdrawal Syndrome (AWS), mental health issues, and a high risk of relapse. Without professional supervision, individuals attempting to quit alcohol face severe physical and psychological consequences, making long-term sobriety more difficult.
The risks of quitting alcohol addiction programs are as follows:
1. Alcohol Withdrawal Syndrome (AWS): Alcohol Withdrawal Syndrome (AWS) is a potentially life-threatening condition that occurs when heavy drinkers abruptly stop consuming alcohol.
Symptoms range from mild anxiety and tremors to severe complications such as seizures and delirium tremens (DTs), which have a mortality rate of up to 37% if untreated, as studied by Alcohol.org. Medically supervised detox programs provide medications like benzodiazepines to manage withdrawal symptoms safely and prevent life-threatening complications.
2. Mental Health Issues: Sudden alcohol cessation triggers or worsens underlying mental health conditions such as depression, anxiety, and psychosis.
Without structured psychological support, individuals experience severe mood swings, suicidal thoughts, or even hallucinations. Addiction programs incorporate cognitive-behavioral therapy (CBT) and psychiatric care to stabilize mental health during recovery.
The prevalence of AUD among persons treated for anxiety disorders is in the range of 20% to 40%, as reported by Lai HMX, Cleary M, Sitharthan T, and Hunt GE. et al. 2015, titled “Prevalence of comorbid substance use, anxiety and mood disorders in epidemiological surveys, 1990–2014: A systematic review and meta-analysis.”
3. High Risk of Relapse: Individuals who quit alcohol without professional help relapse within the first few months.
This is because alcohol cravings, emotional distress, and lack of coping mechanisms make sustained sobriety challenging. Structured treatment programs provide relapse prevention strategies, counseling, and medication-assisted therapy (MAT) to increase the chances of long-term success.
A study by Moos RH, Moos BS. et al. 2006, titled “Rates and predictors of relapse after natural and treated remission from alcohol use disorders,” suggest that between 20% and 95% of people who try to quit alcohol without professional help relapse, depending on the severity of their addiction. While some research estimates that 5% to 45% of untreated individuals achieve some recovery, others suggest that 50% to 80% stay sober over time, meaning a significant portion still struggles with relapse, especially within the first few months of quitting.
4. Social and Emotional Struggles: Alcohol dependence affects personal relationships, and quitting without support leads to feelings of isolation, loneliness, and emotional distress.
Many individuals struggle with guilt, shame, and strained family dynamics, making them more susceptible to relapse. Rehab programs offer group therapy, peer support, and family counseling to help individuals rebuild their social and emotional well-being.
5. Physical Health Complications: Chronic alcohol use leads to liver damage, cardiovascular issues, and weakened immune function.
Stopping alcohol without medical supervision leads to sudden physiological imbalances, increasing the risk of heart arrhythmias, dehydration, and other serious conditions. Medical detox programs monitor vital signs and provide nutritional support to ensure a safe withdrawal process.
Stopping alcohol suddenly, especially without medical help, has serious effects on the heart. Among 1,511,155 hospitalizations for Alcohol Withdrawal Syndrome (AWS) in a study by Thakkar S et al. 2021, titled “Arrhythmias in patients with in-hospital alcohol withdrawal are associated with increased mortality: Insights from 1.5 million hospitalizations for alcohol withdrawal syndrome,” 9.72% (146,825 cases) had arrhythmias, with atrial fibrillation being the most common (66.7%).
6. Lack of Structured Coping Mechanisms: Many individuals use alcohol as a way to cope with stress, trauma, or social anxiety.
Quitting without professional guidance leaves them without effective coping skills, increasing vulnerability to stressors that lead to relapse. Addiction treatment programs teach behavioral strategies, mindfulness, and stress management techniques to build resilience.
What Treatments Are Used in Alcohol Addiction Programs?
The treatments used in alcohol addiction programs include behavioral therapy, medication-assisted treatment, counseling, and support groups, among others. These treatments are designed to help individuals overcome alcohol dependence by addressing both the physical and psychological aspects of addiction. Research-backed approaches ensure that individuals receive comprehensive care to improve long-term recovery outcomes and reduce the risk of relapse.
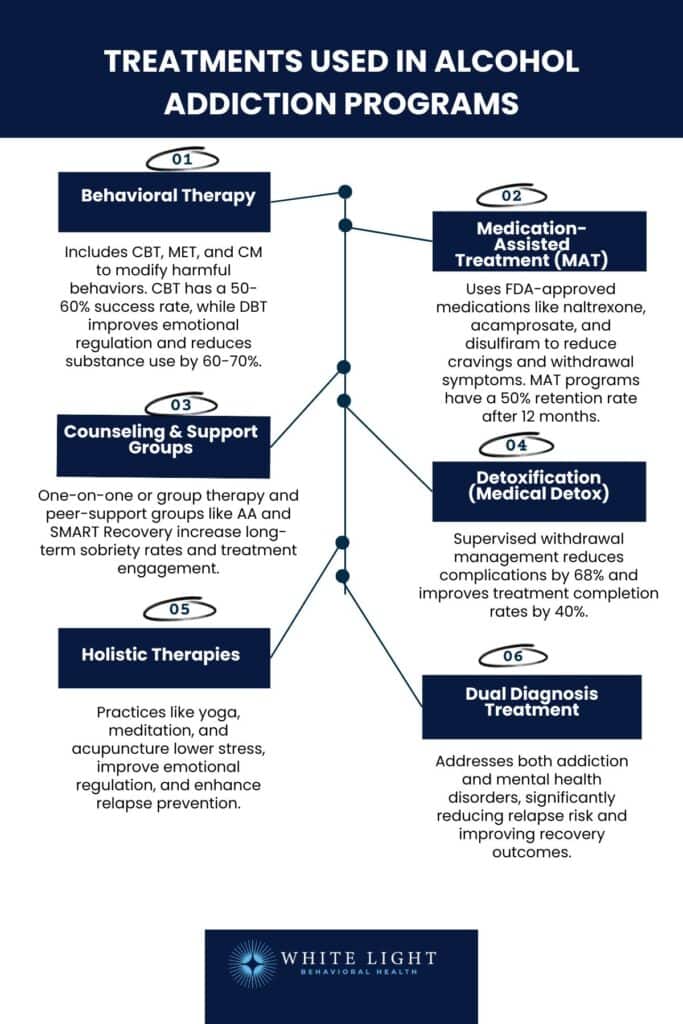
The treatments used in alcohol addiction programs are as follows:
1. Behavioral Therapy: Behavioral therapy is a psychological treatment that helps individuals change harmful drinking behaviors by developing healthier coping mechanisms.
Cognitive Behavioral Therapy (CBT), Motivational Enhancement Therapy (MET), and Contingency Management (CM) are used approaches in alcohol addiction programs. CBT is highly effective, with success rates around 50 to 60% in assisting individuals in reducing or eliminating substance use, according to McHugh RK, Hearon BA, and Otto MW. et al. 2010, titled “Cognitive behavioral therapy for substance use disorders.” These therapies focus on identifying triggers, reshaping negative thought patterns, and reinforcing positive behaviors.
According to clinical research, behavioral therapies are among the most effective interventions for achieving and maintaining long-term sobriety. DBT shows 60 to 70% success rates in improving emotional regulation and reducing substance use, according to a study by Hernandez-Bustamante M, Cjuno J, Hernández RM, and Ponce-Meza JC. et al. 2024, titled “Efficacy of Dialectical Behavior Therapy in the Treatment of Borderline Personality Disorder: A Systematic Review of Randomized Controlled Trials.”
2. Medication-Assisted Treatment (MAT): Medication-assisted treatment involves FDA-approved medications that help reduce alcohol cravings and withdrawal symptoms.
Commonly used medications include naltrexone (reduces cravings), acamprosate (restores brain balance), and disulfiram (causes unpleasant effects when alcohol is consumed). Medication-assisted treatment programs in low- and middle-income countries achieve an average 50% retention rate after 12 months, with wide variation across programs but little difference between those using buprenorphine versus methadone, as studied by Feelemyer J, Des Jarlais D, Arasteh K, Abdul-Quader AS, Hagan H. et al. 2015, titled “Retention of participants in medication-assisted programs in low- and middle-income countries: an international systematic review.” MAT is combined with counseling and behavioral therapies to enhance effectiveness.
3. Counseling and Support Groups: Counseling provides emotional support and guidance through one-on-one or group sessions led by licensed therapists.
Support groups like Alcoholics Anonymous (AA), SMART Recovery, and other peer-led groups offer a sense of community and accountability. These groups follow structured programs that focus on self-reflection, relapse prevention, and emotional healing.
Individuals who participate in support groups have higher chances of maintaining long-term sobriety compared to those who attempt recovery alone.
According to a study by Tracy K, Wallace SP. et al. 2016, titled “Benefits of peer support groups in the treatment of addiction,” support groups for alcohol treatment have been shown to improve substance use reduction, treatment engagement, and self-efficacy while also lowering HIV/HCV risk behaviors though more rigorous studies are needed to isolate their specific impact.
4. Detoxification (Medical Detox): Medical detox is the first step in alcohol addiction treatment, involving the supervised removal of alcohol from the body. Since withdrawal symptoms are severe, including seizures, delirium tremens, and heart complications, medical detox ensures safety through 24/7 monitoring, intravenous fluids, and medications to ease withdrawal effects. A study by Miller PM, Book SW, Stewart SH. et al. 2012, titled “Medical treatment of alcohol dependence: a systematic review,” show that medically supervised detox reduces complications by up to 68% and increases successful completion rates by 40%.
5. Holistic Therapies: Holistic therapies, such as yoga, meditation, acupuncture, art therapy, and nutrition counseling, complement traditional treatments by promoting mental and physical well-being.
These therapies help reduce stress, improve emotional regulation, and enhance overall recovery outcomes. Research by Melemis SM. et al. 2015, titled “Relapse Prevention and the Five Rules of Recovery,” suggests that individuals who engage in holistic treatments experience lower anxiety levels and improved relapse prevention.
6. Dual Diagnosis Treatment: Many individuals with alcohol addiction also suffer from co-occurring mental health disorders such as depression, anxiety, or PTSD. Dual diagnosis treatment addresses both conditions simultaneously, using a combination of therapy, medication, and personalized recovery plans.
A study by the National Institute on Alcohol Abuse and Alcoholism (NIAAA) shows that treating both alcohol addiction and mental health disorders together reduces relapse rates and improves treatment success.
Dual diagnosis treatment significantly reduces relapse rates, as individuals with alcohol use disorder (AUD) and co-occurring mental health conditions, such as depression (27 to 40%), bipolar disorder (42%), or anxiety (20 to 40%), are up to 5 times more likely to have another substance use disorder, highlighting the need for integrated care.
What Is the Cost of Alcohol Addiction Programs?
The cost of an alcohol addiction program is between $250 and $800 per day for outpatient treatment and $6,000 to $30,000 per month for inpatient rehab, depending on the facility, level of care, and duration of treatment. Factors influencing cost include the type of program (inpatient vs. outpatient), medical detox requirements, therapy sessions, and additional services such as dual diagnosis treatment.
Luxury rehab centers with premium amenities exceed $50,000 per month, while state-funded or non-profit programs offer lower-cost or free options. Health insurance covers part or all of the expenses, depending on the plan and provider, under the Affordable Care Act (ACA).
However, individuals without insurance rely on sliding-scale fees, financing plans, or government assistance programs to afford treatment.
What Factors Affect the Cost of Alcohol Addiction Programs?
The factors that affect the cost of an alcohol addiction program include the type of treatment program, duration, medication costs, and facility location, among other variables. Each of these factors plays a paramount role in determining the overall expenses, as different programs offer varying levels of care, resources, and medical supervision.
The factors that affect the cost of an alcohol addiction program are as follows:
1. Type of Treatment Program: The cost of treatment varies significantly based on whether a program is inpatient, outpatient, or detox-focused.
Inpatient rehab is the most expensive, as it includes 24/7 medical care, accommodations, and meals, ranging from $6,000 to $30,000 per month. Outpatient programs are more affordable, costing between $250 and $800 per day, but they require individuals to have a stable home environment for recovery.
Luxury rehab centers with high-end amenities exceed $50,000 per month, while state-funded programs offer free or low-cost options.
2. Duration: The length of time an individual stays in treatment directly affects costs.
Short-term rehab programs lasting 30 days are more affordable than 60- or 90-day programs, but longer durations tend to improve success rates and reduce relapse risk. The cost of extended care increases exponentially, with 90-day inpatient programs exceeding $50,000.
3. Medication Costs: Many alcohol addiction programs involve Medication-Assisted Treatment (MAT), which includes FDA-approved drugs such as naltrexone, disulfiram, and acamprosate.
The cost of these medications varies, with naltrexone injections costing up to $1,300 per month, while generic oral options are more affordable. Individuals requiring detox medications to manage withdrawal symptoms will face additional costs.
4. Location of the Facility: Rehab centers in urban areas, high-cost states (like California and New York), or beachfront/luxury settings tend to be more expensive than those in rural or less populated regions.
Facilities in high-demand areas charge more due to higher operational costs, staff salaries, and property expenses. Traveling out of state for rehab also adds extra expenses for accommodation and transportation.
5. Insurance Coverage: The extent of health insurance coverage greatly influences out-of-pocket expenses for alcohol addiction programs.
Under the Affordable Care Act (ACA), many insurance plans cover addiction treatment, but the level of coverage varies. Some plans cover detox, therapy, and medication, while others require co-pays, deductibles, or out-of-network costs.
Those without insurance need to explore state-funded programs, sliding-scale fees, or financing plans to afford treatment.
6. Additional Services and Amenities: Programs offering specialized services such as dual diagnosis treatment, holistic therapies, or luxury accommodations come at a higher price. Holistic treatments like yoga, acupuncture, or equine therapy add extra costs, while dual diagnosis care, which treats co-occurring mental health disorders, requires specialized professionals, making treatment more expensive.
7. Level of Medical Supervision: Programs that require intensive medical supervision, 24/7 nursing care, or specialized psychiatric support tend to be more costly. Individuals with severe alcohol dependence, chronic health conditions, or a history of relapse require medically supervised detox, which increases treatment costs due to the need for continuous monitoring and emergency care.
How to Choose the Best Rehab Program for Alcohol Addiction?
To choose the best rehab program for alcohol addiction, you must consider the severity of the addiction, the type of treatment required, and personal preferences such as location, cost, and amenities. Inpatient rehab is best for those needing 24/7 medical supervision, while outpatient programs allow individuals to continue daily responsibilities while receiving treatment. Look for evidence-based therapies such as cognitive-behavioral therapy (CBT), medication-assisted treatment (MAT), and holistic approaches. Checking accreditation, staff qualifications, success rates, and insurance coverage also helps in selecting a high-quality program tailored to individual recovery needs.
Are you covered for treatment?
White Light Behavioral Health is an approved provider for Blue Cross Blue Shield and TUFTS, while also accepting many other major insurance carriers.
What Is the First Step in an Alcohol Addiction Program?
The first step in an alcohol addiction program is a comprehensive assessment and detoxification process to evaluate the individual’s physical and mental health, level of alcohol dependence and co-occurring conditions. The assessment includes medical history, substance use patterns, and psychological evaluations to develop a personalized treatment plan.
If necessary, a medically supervised detox process helps manage withdrawal symptoms safely. This step is necessary as it lays the foundation for selecting the right therapy, setting treatment goals, and ensuring a structured recovery path.
What Is the Role of Rehabs in Alcohol Addiction Programs?
The role of rehab in alcohol addiction programs is to provide structured, evidence-based treatment that helps individuals overcome alcohol dependence and build long-term sobriety. Rehabs offer medical supervision for detox, therapy sessions to address psychological aspects of addiction, and life skills training to help individuals reintegrate into society.
Many rehab centers also provide relapse prevention strategies, aftercare planning, and support groups to ensure sustained recovery. By offering a safe, controlled environment, rehab centers help individuals break the cycle of addiction and develop healthier coping mechanisms.
What Role Does Family Play in Alcohol Addiction Recovery?
Family plays an important role in alcohol addiction recovery by providing emotional support, encouragement, and accountability throughout the treatment process. Families participate in family therapy sessions to address dysfunctional dynamics, rebuild trust, and learn how to create a supportive home environment. Educating family members about addiction helps them understand triggers, relapse risks, and effective ways to assist their loved ones without enabling harmful behaviors. A strong family support system improves treatment engagement, reduces stress for the recovering individual, and increases long-term sobriety success rates.
How Do Alcohol Addiction Programs Handle Relapses?
Alcohol addiction programs handle relapses by offering relapse prevention strategies, immediate intervention, and adjusting treatment plans based on the individual’s needs. Many programs emphasize that relapse is not failure but a part of the recovery journey and use it as an opportunity to reinforce coping mechanisms. Behavioral therapies such as cognitive-behavioral therapy (CBT) and motivational enhancement therapy (MET) help individuals identify triggers of relapse and develop stronger resilience. Some programs offer aftercare services, sober living homes, and support groups like Alcoholics Anonymous (AA) to help individuals regain sobriety after a relapse.
Does Insurance Cover Alcohol Addiction Treatment?
Yes, most health insurance covers alcohol addiction treatment under the Affordable Care Act (ACA), but the level of coverage varies. Many insurance providers cover detox, inpatient and outpatient rehab, therapy sessions, and medication-assisted treatment (MAT). However, coverage depends on factors such as network providers, deductibles, co-pays, and pre-authorization requirements. Individuals should check with their insurance provider or use rehab center verification tools to understand their coverage and explore additional financial assistance options if necessary.
Did you know most health insurance plans cover substance use disorder treatment? Check your coverage online now.
Are Medications Used in Alcohol Addiction Programs?
Yes, medications are used in alcohol addiction programs as part of Medication-Assisted Treatment (MAT) to manage withdrawal symptoms, reduce cravings, and prevent relapse. FDA-approved medications include naltrexone (reduces cravings), disulfiram (causes unpleasant effects if alcohol is consumed), and acamprosate (helps maintain abstinence by stabilizing brain chemistry). These medications are combined with behavioral therapy and counseling to improve treatment outcomes and support long-term sobriety.
Can Online Alcohol Addiction Programs Be Effective?
Yes, online alcohol addiction programs can be effective, especially for individuals who cannot attend in-person treatment due to location, work, or personal constraints. These programs provide virtual counseling, therapy sessions, and support groups through telehealth services.
Online cognitive-behavioral therapy (CBT) and virtual support groups like SMART Recovery significantly help individuals manage cravings and maintain sobriety. However, online programs are not suitable for individuals with severe addiction requiring medical detox or intensive supervision.
Which Therapy is Most Suitable for Alcoholism?
Cognitive-behavioral therapy (CBT) is most suitable for alcoholism because it helps individuals identify and change negative thought patterns, develop coping skills, and prevent relapse. CBT is an evidence-based approach that teaches individuals how to manage triggers, stress, and emotional responses that lead to alcohol use. CBT, when combined with medication-assisted treatment (MAT) and support groups, significantly improves long-term recovery outcomes. Other effective therapies include Motivational Enhancement Therapy (MET) and 12-step Facilitation Therapy, both of which help strengthen commitment to sobriety.
Share This Post
















