Addiction: Definition, Types, Causes, Effects, and Treatment

Addiction is a complex condition characterized by compulsive engagement in behaviors or consumption of substances despite harmful consequences. It involves a psychological and physical dependence that impairs an individual’s ability to function in everyday life. Addiction is recognized as both a chronic disease and a serious public health issue.
According to the National Center for Drug Abuse Statistics (NCDAS), nearly 1 million overdose deaths since 2000, and 37.3 million Americans aged 12 and older reported illegal drug use in 2020. Half of all individuals 12 and older have used illicit drugs at least once, and 13.5% used drugs in a month, marking a 3.8% year-over-year increase. The federal government allocated $35 billion for drug control in 2020, yet substance abuse continues to rise.
There are various types of addiction, ranging from substance-related addictions like drugs, alcohol, and nicotine to behavioral addictions such as gambling, internet use, and shopping. These addictions significantly disrupt an individual’s daily functioning, relationships, and overall well-being, manifesting in both physical and psychological symptoms.
The causes of addiction are multifaceted, involving biological, environmental, and psychological factors. Genetic predispositions, brain chemistry imbalances, childhood trauma, and social influences like peer pressure and socioeconomic status all contribute to the development of addiction.
Research by the National Institute on Drug Abuse (NIDA) suggests that genetic factors account for approximately 40–60% of a person’s risk of developing addiction. Psychological conditions like depression and anxiety also heighten the risk of addiction.
The effects of addiction include cognitive impairment, organ damage (such as liver disease), mental health disorders like anxiety and depression, and the deterioration of relationships. Addiction also leads to job loss, financial problems, and even homelessness, all of which worsen the individual’s overall life circumstances.
The treatment options for those battling addiction include medical detoxification, rehabilitation programs (inpatient, outpatient, and partial hospitalization), psychotherapy, medication-assisted treatment (MAT), and support groups like 12-step programs. A combination of these therapies provides the best outcomes, depending on the individual’s needs and addiction severity. According to research from the CDC, 3 out of 4 people (75%) recover from addiction.
What Is Addiction?
Addiction is a chronic disease characterized by compulsive behavior, loss of control, and continued substance use or engagement in harmful activities despite negative consequences. According to the American Society of Addiction Medicine (ASAM), addiction is a primary, chronic disorder affecting brain reward, motivation, and memory circuits.
The Diagnostic and Statistical Manual of Mental Disorders, Fifth Edition (DSM-5), outlines criteria for Substance Use Disorder (SUD), which include impaired control (e.g., unsuccessful attempts to cut down), social impairment, risky use, and pharmacological indicators such as tolerance and withdrawal.
Addiction alters brain circuits, particularly in the prefrontal cortex, which is responsible for decision-making and impulse control, and the limbic system, which regulates emotions and rewards, Volkow ND., et al. 2007, titled “Profound decreases in dopamine release in striatum in detoxified alcoholics: Possible orbitofrontal involvement.” These changes reinforce compulsive behavior, making it difficult for individuals to stop using substances or engaging in addictive activities without professional intervention.
More Resources on Addiction:
According to the National Center for Drug Abuse Statistics (NCDAS), nearly 1 million overdose deaths since 2000, and 37.3 million Americans aged 12 and older reported illegal drug use in 2020. Half of all individuals 12 and older have used illicit drugs at least once, and 13.5% used drugs in a month, marking a 3.8% year-over-year increase. The federal government allocated $35 billion for drug control in 2020, yet substance abuse continues to rise.
Did you know most health insurance plans cover substance use disorder treatment? Check your coverage online now.
Is Addiction a Disease or a Choice?
Yes, addiction is a disease, not just a choice, because it involves chronic changes in brain function that impair self-control and reinforce compulsive behavior. Neurobiological research by Koob GF, Volkow ND. et al. 2016, titled “Neurobiology of addiction: a neurocircuitry analysis,” shows that addiction alters the brain’s reward system, particularly the dopamine pathway, which affects motivation and decision-making.
Opponents argue addiction begins with a choice, but once the brain undergoes neuroadaptations, substance use becomes a compulsive, loss-of-control disorder. While personal responsibility plays a role in seeking treatment, brain chemistry, and genetic factors make addiction a chronic disease, similar to diabetes or heart disease.
How Does Addiction Differ from Dependence?
Addiction differs from dependence by involving compulsive behavior and an inability to stop, whereas dependence is primarily physical adaptation to a substance, according to Medical News Today titled “Addiction vs. dependence: Definitions and differences.” Physical dependence occurs when the body adjusts to a drug, leading to withdrawal symptoms if use stops.
Psychological dependence, or addiction, goes beyond physical symptoms, driving uncontrollable cravings and drug-seeking behavior despite adverse consequences. While dependence occurs with medications like opioids without addiction, addiction reflects a deeper loss of control driven by changes in brain chemistry.
How Does Addiction Develop in the Brain?
Addiction develops in the brain through a complex interplay of neurobiological changes, primarily affecting the brain’s reward system. Repeated substance use overstimulates dopamine, a key neurotransmitter that reinforces pleasurable behaviors. Over time, the brain adapts, reducing dopamine sensitivity, leading to tolerance (needing more substance for the same effect) and cravings.
According to the National Institute for Drug Abuse (NIDA), “The Science of Addiction – Drugs and the Brain,” as addiction progresses, the brain’s prefrontal cortex, responsible for decision-making, weakens, making self-control harder. Research shows that neuroplasticity, the brain’s ability to reorganize, further reinforces addictive behaviors, making quitting difficult without intervention.
What Are the Different Types of Addiction?
The different types of addiction are substance addictions and behavioral (process) addictions. Substance addiction involves dependency on drugs or alcohol, leading to severe health and social consequences.
Process addictions, or behavioral addictions, include compulsive behaviors like gambling, shopping, and internet use, which interfere with daily life and well-being. Both types of addiction cause significant harm and require professional treatment.

The different types of addiction are as follows:
Substance Addiction
Substance addiction, also known as substance use disorder, occurs when individuals develop a physical and psychological dependence on drugs or alcohol. Common substance addictions include alcohol addiction, cocaine addiction, heroin addiction, marijuana addiction, prescription drug addiction, methamphetamine addiction, nicotine addiction, opioid addiction, and benzodiazepine addiction.
This includes alcohol use disorder (AUD), which affects 14.5 million Americans aged 12 and older, leading to severe health risks, according to the Substance Abuse and Mental Health Services Administration (SAMHSA). Nicotine addiction, despite a decline in smoking rates, still impacts 12.5% of U.S. adults as of 2020.
Marijuana use disorder, involving cannabis dependence, affected approximately 4.8 million people in 2020, according to SAMHSA. Opioid use disorder, which includes addiction to prescription opioids and heroin, remains one of the most severe public health crises, affecting 2.7 million people and contributing to high overdose death rates, according to the CDC. Stimulant use disorder, involving drugs like cocaine and methamphetamine, impacted 1.5 million cocaine users and 1.1 million methamphetamine users in 2020, according to SAMHSA. Substance addictions require a combination of medical detox, behavioral therapy, and long-term treatment strategies to prevent relapse and support recovery.
Contact us today to schedule an initial assessment or to learn more about our services. Whether you are seeking intensive outpatient care or simply need guidance on your mental health journey, we are here to help.
Behavioral (Process) Addiction
Behavioral addiction, or process addiction, refers to compulsive behaviors that interfere with a person’s daily life and well-being. Common behavioral addictions include gambling addiction, internet addiction, video game addiction, sex addiction, shopping addiction, food addiction, exercise addiction, work addiction, and social media addiction.
Gambling disorder, characterized by persistent gambling despite negative consequences, affects about 2 million U.S. adults, according to the National Council on Problem Gambling. Internet gaming disorder, where excessive online gaming causes distress, impacts between 0.3% and 1.0% of the population, according to the American Psychiatric Association.
Food addiction, which involves compulsive overeating of highly palatable foods, affects 2.8% of adults, as reported by Wikipedia in the study Addiction. Sex addiction, also known as Compulsive Sexual Behavior Disorder (CSBD), is estimated to impact 3% to 6% of individuals in the U.S. Shopping addiction, or Compulsive Buying Disorder (CBD), has a 5.8% lifetime prevalence in the U.S., according to a study published in World Psychiatry. These behavioral addictions, though different from substance use disorders, lead to significant psychological, social, and financial consequences, requiring therapy and professional intervention.
What Causes Addiction?
Addiction is caused by a combination of biological, environmental, and psychological factors that influence brain function and behavior. Biological factors, such as genetics and neurochemical imbalances, make some individuals more vulnerable to addiction by altering dopamine regulation and impulse control, with research by Ducci F, Goldman D. et al. 2012, titled “The genetic basis of addictive disorders,” suggesting that 40-60% of addiction risk is attributable to genetic factors.
Environmental factors, including exposure to substance use, peer pressure, trauma, and socioeconomic conditions, shape addictive behaviors. Psychological factors, such as stress, mental health disorders (like depression or anxiety), and coping mechanisms further contribute to addiction by reinforcing substance use or compulsive behaviors as a form of relief. Research by CAMH titled “Mental Illness and Addiction: Facts and Statistics” indicates that individuals with mental health disorders are about twice as likely to develop substance use disorders as those without.
A study by He J et al. 2022, titled “Does Childhood Adversity Lead to Drug Addiction in Adulthood? A Study of Serial Mediators Based on Resilience and Depression,” reveals that individuals with high ACE scores are 4 to 12 times more likely to struggle with addiction due to the stress and coping mechanisms developed in response to early trauma.
How Do Genetics and Biology Influence Addiction?
Genetics and biology influence addiction by shaping an individual’s vulnerability to substance use disorders through hereditary risk, brain chemistry, and genetic variations. Research by the National Institute on Drug Abuse (NIDA) suggests that genetic factors account for approximately 40–60% of a person’s risk of developing addiction. Variations in dopamine receptors (such as the DRD2 gene) affect the brain’s reward system, making some individuals more prone to compulsive behavior and substance dependence.
Twin studies by Ducci F, Goldman D. et al. 2012, titled “The genetic basis of addictive disorders,” provide strong evidence of genetic influence, showing that if one identical twin has a substance use disorder, the other twin has a significantly higher likelihood of developing addiction compared to fraternal twins. While genetics increase susceptibility, environmental and psychological factors also play important roles in addiction development.
What Environmental and Social Factors Lead to Addiction?
Environmental and social factors that lead to addiction include peer pressure, family dynamics, socioeconomic status, and childhood trauma, all of which shape an individual’s risk for substance use disorders. Peer pressure, especially during adolescence, encourages experimentation with drugs or alcohol, increasing the likelihood of addiction.
Family dynamics, such as parental substance use or lack of support, also shape behavioral patterns. Socioeconomic status, including poverty and limited access to education or healthcare, heighten stress and make individuals more vulnerable to substance use as a coping mechanism.
A study by He J et al. 2022, titled “Does Childhood Adversity Lead to Drug Addiction in Adulthood? A Study of Serial Mediators Based on Resilience and Depression,” found that individuals with high ACE scores are 4 to 12 times more likely to develop addiction.
This increased risk is linked to the stress and maladaptive coping mechanisms formed in response to early trauma.
According to the Centers for Disease Control and Prevention (CDC), individuals with four or more ACEs are two to four times more likely to engage in heavy substance use later in life. Addressing these environmental and social risk factors is important for effective addiction prevention and intervention.
What Psychological Conditions Increase the Risk of Addiction?
Psychological conditions that increase the risk of addiction include anxiety, depression, PTSD, and other mental health disorders, as these conditions drive individuals to use substances as a form of self-medication. People struggling with mental health issues turn to drugs or alcohol to manage their symptoms, which leads to the development of substance use disorders (SUDs).
The co-occurring disorders that increase the risk of addiction are as follows:
- Anxiety Disorders: Individuals with anxiety are at higher risk for addiction due to the tendency to use substances like alcohol or benzodiazepines to reduce overwhelming feelings of worry and fear. A study by the National Institute on Drug Abuse (NIDA), “Co-Occurring Disorders and Health Conditions,” shows that about 20% of people with anxiety disorders also have a co-occurring substance use disorder.
- Depression: Major depressive disorder (MDD) is closely linked with addiction, as individuals use drugs or alcohol to alleviate symptoms of sadness, hopelessness, and fatigue. Depression is reported by 40-60% of individuals with addiction, as studied by Grant, B. F., Stinson, F. S., Dawson, D. A., et al. 2004, titled “Prevalence and co-occurrence of substance use disorders and independent mood and anxiety disorders: Results from the National Epidemiologic Survey on Alcohol and Related Conditions.”
- Post-Traumatic Stress Disorder (PTSD): Those with PTSD self-medicate using substances to cope with flashbacks, nightmares, or hyperarousal.
Research by The Substance Abuse and Mental Health Services Administration (SAMHSA) shows that up to 50% of individuals with PTSD also struggle with substance use disorders.
- Bipolar Disorder: People with bipolar disorder are at a higher risk for addiction, especially during manic or depressive episodes when impulsivity and risky behaviors are more prevalent. A study by HelpGuide titled “Dual Diagnosis: Substance Abuse and Mental Health” suggests that 30% of individuals with bipolar disorder have a co-occurring substance use disorder.
- Attention-Deficit/Hyperactivity Disorder (ADHD): Individuals with ADHD use substances to improve concentration or calm hyperactivity, contributing to a higher likelihood of addiction.
Research by the National Institute of Mental Health (NIMH) indicates that about 15-25% of people with ADHD also experience substance abuse issues.
Rediscover Life at White Light Behavioral Health
Get the compassionate support you deserve. We're here to help you reclaim joy, wellness, and a brighter future.
Our Facility
What Are the Risk Factors for Addiction?
The risk factors for addiction are a combination of biological, environmental, and psychological influences that increase an individual’s vulnerability to developing substance use disorders. These factors make it harder to resist the urge to use drugs or alcohol, leading to compulsive behavior and addiction.
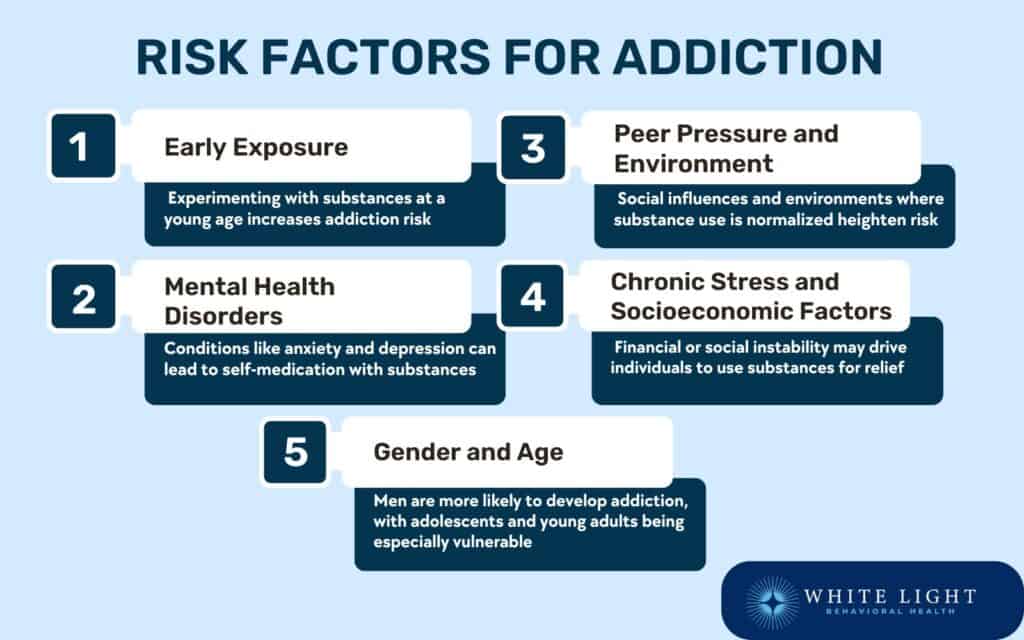
The risk factors for addiction are as follows:
- Early Exposure to Drugs or Alcohol: Early experimentation with drugs or alcohol, especially during adolescence, increases the likelihood of developing addiction later in life. The younger the age at which substance use begins, the more likely it is to become habitual and progress into a disorder.
This early exposure disrupts normal brain development and leads to long-term vulnerability.
- Mental Health Disorders: Psychological conditions like anxiety, depression, and PTSD significantly increase addiction risk as individuals use substances as a form of self-medication to cope with distressing symptoms. People with mental health disorders are more likely to develop substance use disorders due to the overlap in brain circuits that regulate both emotions and addiction, according to research by CAMH titled “Mental Illness and Addiction: Facts and Statistics.”
- Peer Pressure and Social Environment: Peer pressure and social influences, particularly during adolescence, increase the likelihood of substance use.
People in environments where drug use is normalized or encouraged are at higher risk of developing addiction. Social support and positive role models are key protective factors against the development of substance use disorders.
- Chronic Stress and Socioeconomic Factors: Chronic stress due to financial hardship, job insecurity, or social instability increases addiction risk by prompting individuals to seek relief through drugs or alcohol.
Socioeconomic factors, such as living in poverty, exacerbate stress, reduce access to education and healthcare, and limit opportunities for positive social engagement, increasing vulnerability to substance abuse.
- Gender and Age: Gender and age also influence addiction risk. Men are more likely to develop addiction than women, though women tend to experience more severe physical and mental health consequences from substance use.
Adolescence and young adulthood are particularly high-risk periods for developing addiction due to changes in brain development, peer influences, and experimentation with substances.
Who Is Most Vulnerable to Addiction?
Individuals with a family history of addiction, mental health disorders, or those exposed to high-stress environments are most vulnerable to addiction. Adolescents are at increased risk due to the ongoing development of brain regions involved in decision-making and impulse control.
These factors contribute to a higher susceptibility to substance use and addiction.
The following individuals are most vulnerable to addiction:
- Adolescents and Young Adults: Adolescent brain development is a key factor in vulnerability to addiction. The brain regions responsible for impulse control and decision-making, like the prefrontal cortex, are not fully developed until the mid-20s, making teens and young adults more susceptible to risky behaviors, including substance use.
Peer influence and experimentation also increase addiction risk during these years.
- Individuals with Mental Health Disorders: People with co-occurring disorders, such as anxiety, depression, or PTSD, are at higher risk for addiction as they use substances to self-medicate their symptoms. This leads to a cycle of substance abuse that exacerbates both the mental health disorder and the addiction.
- People with a Family History of Addiction: Genetic factors significantly contribute to addiction risk.
Individuals with a family history of addiction are more likely to develop similar behaviors due to shared genetic traits that affect dopamine pathways and the brain’s reward system, making them more susceptible to developing substance use disorders.
- Individuals in High-Stress Environments: People who experience chronic stress, whether due to financial strain, trauma, or socioeconomic instability, are at a higher risk for stress-related addiction. Stress triggers substance use as a coping mechanism, increasing the likelihood of addiction.
Those living in environments where substance abuse is normalized or prevalent are more likely to develop dependency.
How Does Early Exposure Increase Addiction Risk?
Early exposure increases addiction risk by disrupting normal brain development and altering the brain’s reward system, making individuals more susceptible to substance dependence later in life. The adolescent brain is particularly vulnerable to substance use, as it is still undergoing necessary developmental changes. Early substance use rewires the brain, affecting areas involved in decision-making, impulse control, and reward processing, leading to a higher likelihood of developing addiction.
Early exposure increases addiction risk in the following ways:
- Rewiring the Brain’s Reward System: Early substance use disrupts the brain’s dopamine pathways, which are responsible for feelings of pleasure and reward. The brain becomes dependent on the substance to release dopamine, making it harder to experience pleasure from normal, non-substance-related activities.
Research by the National Institute on Drug Abuse (NIDA) has shown that adolescents who begin using substances like alcohol or marijuana are more likely to have altered brain chemistry, leading to increased vulnerability to addiction.
- Increased Impulse Control and Risk-Taking Behavior: The prefrontal cortex, which is responsible for impulse control, is not fully developed during adolescence. Early exposure to drugs or alcohol impairs this development, leading to heightened impulsivity and risky behaviors.
Winters KC, Arria A., et al. 2011, in their study titled “Adolescent Brain Development and Drugs,” have shown that adolescents who experiment with substances are more likely to engage in risky behaviors and have a reduced ability to make sound judgments.
- Early Exposure Increases Dependence: When individuals begin using substances at a young age, their brain circuits become accustomed to the substance, increasing the likelihood of dependence. Early use leads to tolerance and withdrawal symptoms, reinforcing the cycle of addiction.
According to the National Institute on Drug Abuse (NIDA), individuals who start using drugs or alcohol before the age of 18 are at a significantly higher risk of developing addiction in adulthood.
- Greater Risk of Mental Health Disorders: Early exposure to substances is associated with an increased risk of developing mental health disorders like depression or anxiety, which drive continued substance use as a form of self-medication. This combination of mental health issues and substance use creates a cycle that is harder to break and increases the risk of long-term addiction.
What Are the Effects of Addiction?
The effects of addiction include physical health, mental well-being, relationships, and social functioning. In the short term, addiction leads to cognitive impairment, memory loss, and impaired decision-making.
Over time, long-term addiction causes physical health deterioration, such as liver damage, heart disease, respiratory issues, and neurological problems.
Addiction also strains relationships with family, friends, and colleagues, leading to isolation, job loss, and financial instability. On a societal level, addiction contributes to crime, homelessness, and increased healthcare costs. For example, in the U.S., opioid overdose deaths reached over 80,000 in 2021, highlighting the severe toll of addiction on public health as reported by the Centers for Disease Control and Prevention (CDC) in “U.S. Overdose Deaths In 2021 Increased Half as Much as in 2020 – But Are Still Up 15%.” Addiction exacerbates existing mental health disorders, leading to a dangerous cycle of dependence and emotional distress.
How Does Addiction Impact Brain Function?
Addiction impacts brain function by disrupting normal brain circuits, particularly those involved in dopamine regulation, decision-making, and impulse control. The brain’s reward system, which relies on dopamine to experience pleasure and motivation, is hijacked by addictive substances, leading to dopamine dysregulation.
This causes the brain to become reliant on the substance for dopamine release, reducing its ability to generate pleasure naturally. Over time, the brain adapts to the constant presence of the drug, a process called neuroplasticity, leading to tolerance and increased substance use.
Research by SAMHSA titled “The Neurobiology Of Substance Use, Misuse, And Addiction” shows that chronic addiction leads to long-term deficits in brain chemistry, with some effects persisting even after recovery.
Addiction also impairs decision-making and impulse control by affecting the prefrontal cortex, the region responsible for higher-order functions such as judgment, planning, and self-regulation. Long-term substance use causes significant brain damage, particularly in areas that govern cognition and behavior. For example, chronic alcohol use shrinks the prefrontal cortex and impairs cognitive function, as studied by Abernathy K, Chandler LJ, Woodward JJ. et al. 2010, titled “Alcohol and the prefrontal cortex.”
Research on opioid addiction by Kibaly C, Xu C, Cahill CM, Evans CJ, Law PY., et al. 2019, titled “Non-nociceptive roles of opioids in the CNS: opioids’ effects on neurogenesis, learning, memory, and effect” has demonstrated that long-term opioid use causes lasting changes in brain structure and function, leading to memory deficits and reduced cognitive abilities. These brain changes make it increasingly difficult for individuals to quit using substances, even when they desire to, and lead to persistent cognitive impairment long after cessation of use.
Are you covered for treatment?
White Light Behavioral Health is an approved provider for Blue Cross Blue Shield and TUFTS, while also accepting many other major insurance carriers.
Check Coverage Now!What Are the Physical and Mental Health Effects of Addiction?
The physical and mental health effects of addiction are physical health deterioration, such as cardiovascular issues and liver damage, and mental health disorders like anxiety and depression, and the development of co-occurring disorders. These wide-ranging effects significantly impair overall well-being. Both short-term and long-term substance abuse have lasting consequences on the brain and body.
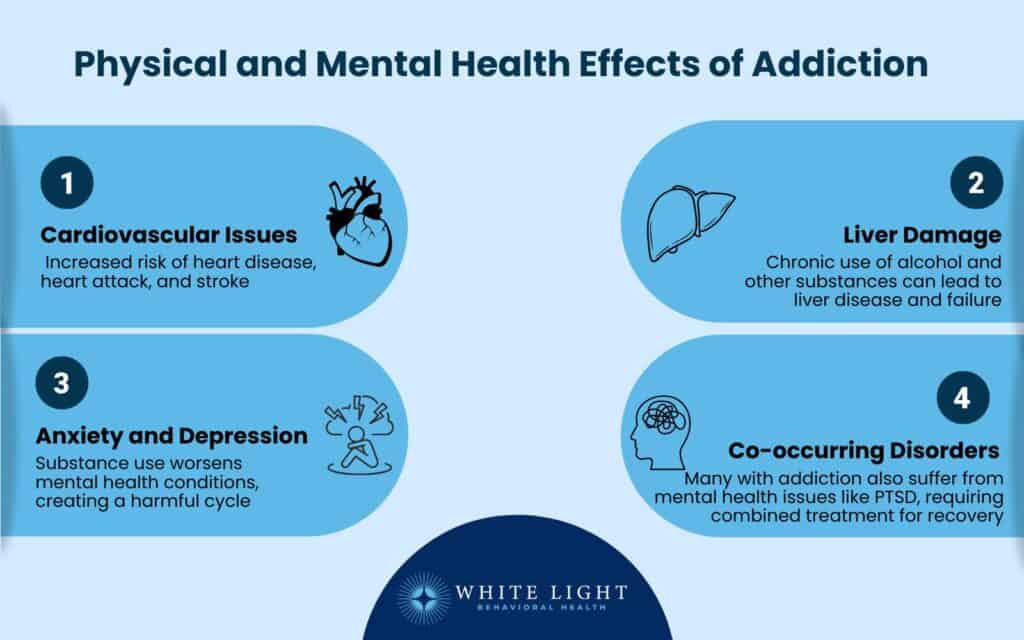
The physical and mental health effects of addiction are as follows:
- Cardiovascular Issues: Addiction strains the heart and blood vessels, leading to heart disease and an increased risk of heart attack and stroke. Stimulant drugs, such as cocaine and methamphetamine, elevate blood pressure, cause irregular heart rhythms, and damage heart tissue.
Long-term use of these substances, like cocaine, is associated with an increased risk of cardiovascular disease and related complications, according to a study by Tim, S.T. & Park, T. et al. 2019, titled “Acute and chronic effects of cocaine on cardiovascular health.”
- Liver Damage: Chronic alcohol use and other substances lead to severe liver damage, such as cirrhosis, fatty liver disease, and liver failure. The liver is responsible for detoxifying the body, and prolonged substance use overwhelms its capacity, leading to liver damage and increasing the risk of liver cancer.
About 50% of heavy alcohol users develop some form of liver disease, according to a study by Osna NA, Donohue TM Jr, and Kharbanda KK. et al. 2017, titled “Alcoholic Liver Disease: Pathogenesis and Current Management.”
- Anxiety and Depression: Addiction is strongly linked with anxiety and depression, both of which worsen due to substance use. Substances like alcohol, opioids, and stimulants alter brain chemistry and exacerbate emotional distress, making it harder for individuals to cope with daily life.
Self-medication through substances becomes a cycle where mental health symptoms lead to more substance use, and substance use worsens mental health.
- Co-occurring Disorders: Many individuals with addiction also suffer from co-occurring disorders, which means they experience both substance use disorders and mental health conditions. For example, people with PTSD use drugs or alcohol to numb emotional pain, which results in a combination of psychological and substance-related problems.
The co-occurrence of these disorders makes treatment more complex, as both need to be addressed simultaneously for effective recovery.
How Does Addiction Affect Relationships and Society?
Addiction affects relationships and society by causing family breakdown, job loss, financial strain, increased crime rates, and homelessness. Substance use disorders lead to strained relationships, as individuals struggling with addiction neglect responsibilities, engage in dishonesty, or exhibit erratic behavior, leading to divorce, child neglect, or domestic conflicts.
In the workplace, addiction contributes to poor job performance, absenteeism, and higher unemployment rates, with approximately 9% of full-time employees in the U.S. reporting substance use disorders, according to the National Safety Council, “Substance Use Disorders by Occupation.” Financial strain is another major consequence, as individuals deplete savings or accumulate debt to sustain their addiction.
On a societal level, addiction is linked to higher crime rates, with drug-related arrests making up 26% of all arrests in the U.S., as reported by the FBI Uniform Crime Report titled “Drugs and Crime Facts.” Substance abuse contributes to homelessness, as many individuals struggling with addiction lose stable housing due to financial instability or legal issues. A report by the National Coalition for the Homeless states that 38% of homeless individuals suffer from alcohol dependency, while 26% struggle with drug addiction.
How is Addiction Diagnosed?
Addiction is diagnosed by medical professionals using clinical assessments, screening tools, and the DSM-5 criteria for substance use disorder (SUD). The Diagnostic and Statistical Manual of Mental Disorders (DSM-5) outlines 11 criteria for addiction diagnosis, including loss of control, compulsive behavior, cravings, withdrawal symptoms, and continued substance use despite negative consequences. A person meeting 2–3 criteria is classified as having a mild disorder, 4–5 criteria indicate a moderate disorder and 6 or more signify a severe substance use disorder.
Medical professionals assess addiction severity through clinical assessments, such as the Alcohol Use Disorders Identification Test (AUDIT) and the Drug Abuse Screening Test (DAST). They also conduct physical exams, patient interviews, and psychological evaluations to determine the extent of substance dependence and its impact on daily life.
Additional diagnostic tools like toxicology screenings (urine or blood tests) help confirm substance use. Comprehensive evaluations allow healthcare providers to develop personalized treatment plans, ensuring proper intervention for individuals struggling with addiction.
What Are the Best Treatment Options for Addiction?
The best treatment options for addiction are medical detoxification, rehabilitation programs, psychotherapy, medication-assisted treatment (MAT), 12-step programs, holistic therapies, and dual diagnosis treatment. These approaches help individuals overcome substance use disorder by addressing physical dependence, behavioral patterns, and underlying mental health conditions. According to research from the CDC, 3 out of 4 people (75%) recover from addiction.

The best treatment options for addiction are as follows:
1. Medical Detoxification
Medical detoxification is the first step in addiction treatment, where individuals undergo supervised withdrawal from addictive substances in a controlled medical environment.
Detox helps manage withdrawal symptoms and reduces the risk of complications through medications, hydration therapy, and medical monitoring. It is important for individuals with severe substance dependence, as sudden cessation leads to life-threatening withdrawal symptoms.
The effectiveness of detoxification significantly improves when paired with continuous therapy and support. A study by Bailey GL, Herman DS, and Stein MD et al. 2013, titled “Perceived Relapse Risk and Desire for Medication-Assisted Treatment Among Persons Seeking Inpatient Opiate Detoxification,” found that 70-80% of individuals who complete detox successfully begin their recovery journey with a lower likelihood of relapse.
The medical detox Is done in the following steps:
- Evaluation: Medical professionals assess the patient’s physical health, substance use history, and co-occurring disorders to determine a personalized detox plan.
- Stabilization: Patients receive medications, IV fluids, and nutritional support to manage withdrawal symptoms and ensure a safe detox process.
- Withdrawal Symptom Management: Physicians administer FDA-approved medications like benzodiazepines, methadone, or buprenorphine to alleviate withdrawal discomfort and cravings.
- Transition to Treatment: After detox, patients are encouraged to continue rehabilitation programs or therapy to maintain long-term sobriety and prevent relapse.
Did you know most health insurance plans cover substance use disorder treatment? Check your coverage online now.
2. Rehabilitation Programs
Rehabilitation programs provide structured treatment to help individuals recover from addiction through therapy, medical care, and relapse prevention strategies. These programs vary in intensity and duration based on the individual’s needs.
Success rates differ based on the type of treatment, with inpatient programs achieving a 60-70% success rate, while outpatient programs report a 50-60% success rate in maintaining sobriety after one year. A study by McCarty D et al. 2014, titled “Substance Abuse Intensive Outpatient Programs: Assessing the Evidence,” emphasizes these variations in treatment effectiveness.
The different rehab types are as follows:
- Inpatient Rehabilitation: Inpatient rehab requires individuals to stay in a residential treatment facility where they receive 24/7 medical and psychological support. This highly structured environment includes individual and group therapy, medication management, and life skills training to promote long-term sobriety.
Patients benefit from a drug-free setting, constant supervision, and an immersive recovery experience, reducing the risk of relapse. However, inpatient programs are costly and require individuals to take time off from work, school, or family obligations.
- Partial Hospitalization Program (PHP): A Partial Hospitalization Program (PHP) offers intensive treatment without requiring full-time residence.
Patients attend structured therapy sessions, medical check-ups, and psychiatric care during the day but return home at night. PHP is a middle ground between inpatient and outpatient care, making it ideal for individuals who need comprehensive treatment but have a stable home environment.
It includes behavioral therapy, medication management, and relapse prevention strategies, allowing individuals to transition to everyday life while receiving high-level support gradually.
- Intensive Outpatient Program (IOP): An Intensive Outpatient Program (IOP) provides structured therapy multiple times a week, allowing individuals to maintain work, school, and family responsibilities while receiving necessary support. IOP focuses on relapse prevention, coping strategies, and mental health management through individual counseling, group therapy, and educational workshops.
While less restrictive than inpatient rehab, IOPs still provide a strong support system and accountability, making them effective for individuals who need flexibility but still require professional guidance.
3. Psychotherapy
Psychotherapy helps individuals address the psychological and behavioral aspects of addiction by modifying negative thought patterns and developing healthy coping mechanisms.
It is a core component of addiction recovery and relapse prevention.
The types of psychotherapy for addiction treatment are as follows:
- Cognitive Behavioral Therapy (CBT): CBT helps individuals identify and change destructive thought patterns that lead to substance abuse, with success rates around 50-60% in assisting individuals in reducing or eliminating substance use, according to McHugh RK, Hearon BA, Otto MW. et al. 2010, titled “Cognitive behavioral therapy for substance use disorders.”
- Dialectical Behavior Therapy (DBT): DBT focuses on emotional regulation and distress tolerance, making it beneficial for individuals with dual diagnoses, such as addiction and borderline personality disorder. DBT shows 60-70% success rates in improving emotional regulation and reducing substance use, according to a study by Hernandez-Bustamante M, Cjuno J, Hernández RM, and Ponce-Meza JC. et al. 2024, titled “Efficacy of Dialectical Behavior Therapy in the Treatment of Borderline Personality Disorder: A Systematic Review of Randomized Controlled Trials.”
- Eye Movement Desensitization and Reprocessing (EMDR): EMDR is used to treat trauma-related addictions, helping individuals process distressing memories linked to substance use. Research by Texas Tech University shows EMDR significantly reduces PTSD symptoms; approximately 84-90% of single-trauma victims no longer have PTSD after just three 90-minute sessions.
This approach helps clients suffering from addiction achieve symptom relief and emotional healing more rapidly than traditional methods.
- Family Therapy: Family therapy addresses dysfunctional family dynamics and improves communication between individuals in recovery and their loved ones. It helps reduce enabling behaviors and strengthen support systems.
4.
Medication-Assisted Treatment (MAT)
Medication-assisted treatment (MAT) combines FDA-approved medications with behavioral therapy to treat substance use disorders. MAT is particularly effective for opioid and alcohol addiction, as it reduces withdrawal symptoms, cravings, and relapse risks.
Medication-assisted treatment (MAT) has been shown to reduce mortality rates by 50% among individuals with opioid addiction, leading to significantly better recovery outcomes. A 2023 study by Bahrami K, Kuo YF, Digbeu B, and Raji MA examined the link between MAT and the risk of drug overdose-related hospitalizations or emergency room visits, highlighting its effectiveness in preventing severe complications in their study titled “Association of Medication-Assisted Therapy and Risk of Drug Overdose-Related Hospitalization or Emergency Room Visits in Patients With Opioid Use Disorder.”
A systematic review conducted by Timko C et al. 2016 analyzed 55 studies on MAT retention rates between 2010 and 2014 in a paper titled “Retention in medication-assisted treatment for opiate dependence: A systematic review.” The review found considerable variability in retention rates across different follow-up periods in randomized controlled trials, ranging from 19–94% at 3 months, 46–92% at 4 months, 3–88% at 6 months, and 37–91% at 12 months.
The following medications are used for the treatment of addiction:
- Methadone: Methadone is a long-acting opioid agonist that reduces cravings and withdrawal symptoms. Research by the National Institute on Drug Abuses shows that methadone reduces opioid-related mortality by 50% or more.
Patients on methadone had 33 percent fewer opioid-positive drug tests and were 4.44 times more likely to stay in treatment compared to controls.
- Buprenorphine (Suboxone): Buprenorphine is a partial opioid agonist that blocks the effects of opioids while preventing withdrawal symptoms. A 2012 study by Ling W. et al. 2012 titled “Buprenorphine implant for opioid addiction” demonstrated the effectiveness of buprenorphine implants in treating opioid addiction.
Approximately 50% of individuals achieved successful opioid-use outcomes during 12 weeks of sustained treatment.
- Naltrexone: Naltrexone is an opioid antagonist that prevents the euphoric effects of drugs like heroin and alcohol, reducing relapse rates. A 2008 study by Anton RF. et al. 2008, titled “Naltrexone for the management of alcohol dependence,” found that naltrexone (100 mg daily for 16 weeks) was more effective than a placebo in treating alcohol dependence, even without behavioral therapy.
Patients receiving naltrexone had a higher percentage of abstinent days (80.6% vs. 75.1%) and a lower risk of heavy drinking days (66.2% vs.
73.1%).
- Disulfiram (Antabuse): Disulfiram is used for alcohol addiction. It creates unpleasant effects like nausea if alcohol is consumed.
A 2014 study by Skinner MD et al. 2014, “Disulfiram efficacy in the treatment of alcohol dependence: a meta-analysis,” found that disulfiram was more effective than a placebo in treating alcohol dependence. In open-label trials, disulfiram showed a significant benefit compared to controls.
It also worked better than naltrexone and acamprosate, making it a strong treatment option for alcohol dependence. However, blind trials did not show the same level of effectiveness.
5.
12-Step Programs
12-step programs like Alcoholics Anonymous (AA) and Narcotics Anonymous (NA) provide a structured, peer-supported approach to addiction recovery. These programs emphasize personal responsibility, spiritual growth, and community support to help individuals maintain long-term sobriety.
Key Steps in 12-Step Programs are as follows:
- Admitting powerlessness over addiction
- Believing in a higher power (not necessarily religious)
- Making a moral inventory of past mistakes
- Making amends with those harmed
- Helping others in recovery
6. Holistic Therapies
Holistic therapies focus on mind-body wellness and aim to treat addiction by improving mental, physical, and emotional health. These therapies complement traditional treatment approaches by reducing stress, cravings, and relapse risks.
The following holistic approaches are used to treat addiction:
- Yoga & Meditation: These practices promote mindfulness, stress reduction, and emotional balance, helping individuals develop healthier coping strategies. A National Center for Complementary and Integrative Health study shows that yoga reduces cravings and improves mood during recovery.
- Acupuncture: Acupuncture is a technique where thin needles are inserted into specific areas of the body to encourage healing and restore balance in the body’s energy flow.
It is commonly used to alleviate withdrawal symptoms, including anxiety, insomnia, and cravings, particularly in the treatment of opioid and nicotine addiction. A study by Wild B. et al. 2020, titled “Acupuncture in persons with an increased stress level—Results from a randomized-controlled pilot trial,” found that acupuncture significantly reduces stress and promotes relaxation.
- Nutritional Therapy: Nutritional Therapy aids recovery by restoring the body’s nutrient levels, which are depleted during substance abuse.
Proper nutrition helps improve brain function, stabilize mood, and boost energy, supporting both physical and mental health during recovery. A balanced diet also enhances detoxification and reduces cravings, promoting long-term healing.
Contact us today to schedule an initial assessment or to learn more about our services.
Whether you are seeking intensive outpatient care or simply need guidance on your mental health journey, we are here to help.
7. Dual Diagnosis Treatment
Dual diagnosis treatment is designed for individuals with co-occurring mental health disorders and addiction. Many people with depression, PTSD, anxiety, or bipolar disorder turn to substances as a form of self-medication, leading to worsened symptoms and addiction.
Integrated treatment is necessary for long-term recovery, as addressing only one condition increases the likelihood of relapse. A study by the National Institute on Drug Abuse indicates that nearly 50% of individuals with a substance use disorder also have a co-occurring mental illness. Dual diagnosis programs provide psychiatric care, therapy, and medication management to ensure a comprehensive recovery approach.
Is Addiction Treatment Covered by Insurance in the U.S.?
Yes, addiction treatment is covered by insurance in the U.S. under the Affordable Care Act (ACA), which mandates that substance use disorder (SUD) treatment is an important health benefit. Medicaid, Medicare, and private insurance plans cover detox, rehabilitation programs, medication-assisted treatment (MAT), and therapy. Coverage details of each insurance vary based on the provider and plan.
Accepted insurance types are as follows:
- Medicaid & Medicare (state-specific eligibility and coverage)
- Employer-Sponsored Health Insurance
- Marketplace/ACA Plans
- Private Health Insurance (e.g., Blue Cross Blue Shield, Cigna, Aetna, UnitedHealthcare)
- Military Insurance (TRICARE)
Can You Recover From Addiction Without Professional Help?
Yes, you can recover from addiction without professional help, but the process is challenging. Self-recovery requires strong willpower, personal motivation, and a solid support system, such as family and friends.
However, the risk of relapse is high without professional guidance, and the journey is isolating. While some individuals are successful in managing their addiction through willpower alone, professional intervention is necessary when addiction is severe or when co-occurring mental health disorders, withdrawal symptoms, or cravings become overwhelming.
The pros and cons of self-recovery are as follows:
- Pros: It offers independence, personal growth, and a sense of achievement. It is cost-effective if professional treatment is not accessible.
- Cons: The risk of relapse is high, and without proper support or therapy, individuals struggle with underlying psychological issues.
Professional intervention is necessary for those with long-term or severe addiction.
How to Prevent Relapse Effectively?
To prevent relapse effectively, it is important to develop a strong foundation of coping skills, build a supportive network, and identify and manage triggers. Preventing relapse requires ongoing commitment and maintaining a focus on recovery, as triggers such as stress, social situations, and emotional struggles lead to setbacks.
To prevent relapse effectively, the following strategies are employed:
- Building Coping Skills: Developing effective coping strategies helps individuals manage stress, emotions, and cravings without turning to substance use. This includes mindfulness, deep breathing, and problem-solving techniques.
- Creating a Support System: Having a solid support system, including family, friends, or support groups, provides emotional encouragement and accountability, which are necessary for long-term recovery.
- Identifying and Avoiding Triggers: Identifying and avoiding situations, environments, or people that trigger a desire to use substances is required.
This requires self-awareness and the ability to set boundaries.
- Engaging in Ongoing Therapy: Continuing therapy, whether individual or group, helps reinforce recovery goals, provides emotional support, and allows individuals to address unresolved issues contributing to addiction.
- Maintaining a Healthy Lifestyle: Exercise, balanced nutrition, and adequate sleep improve overall well-being and reduce stress, which lowers the risk of relapse.
What Are the Most Common Relapse Triggers?
The most common relapse triggers are stress, social circles, emotional distress, and environmental factors. These triggers cause individuals to feel overwhelmed or vulnerable, which leads to a lapse in recovery.
The most common relapse triggers are as follows:
- Stress: High levels of stress from work, relationships, or life challenges make people feel anxious or out of control, which increases the temptation to turn to substances for relief. Stress management techniques, such as mindfulness or relaxation exercises, are important for coping with these situations.
- Social Circles: Spending time with individuals who use substances or who do not support recovery increases the risk of relapse.
Social pressure or simply being in familiar environments where substance use is common tempts someone to relapse. Healthy, supportive relationships are key to recovery.
- Emotional Distress: Feelings of sadness, anger, or anxiety lead individuals to seek substances as a form of self-medication.
Learning to cope with emotions in a healthy way through therapy or other coping strategies is necessary to avoid relapse.
- Environmental Triggers: Certain environments, such as bars, parties, or areas where drug use is prevalent, act as powerful triggers. Being mindful of these environments and avoiding them when possible helps reduce the likelihood of relapse.
Rediscover Life at White Light Behavioral Health
Get the compassionate support you deserve.
We're here to help you reclaim joy, wellness, and a brighter future.
Our Facility
How Can You Rewire Your Brain After Addiction?
You can rewire your brain after addiction by leveraging the brain’s neuroplasticity to create new, healthier neural pathways. Neuroplasticity is the brain’s ability to adapt and reorganize itself by forming new connections in response to experiences. Engaging in specific activities and lifestyle changes helps restore brain function and strengthen the neural pathways supporting positive behaviors and coping mechanisms.
You can rewire your brain after addiction by following the below-mentioned steps:
- Engage in Therapy: Cognitive-behavioral therapy (CBT) and other therapeutic approaches help identify and change negative thought patterns, replacing them with healthier alternatives. Therapy also supports emotional regulation, helping you navigate triggers and challenges in recovery.
- Exercise Regularly: Physical activity has been shown to stimulate the release of dopamine and endorphins, chemicals that improve mood and motivation.
According to a study by Lin TW, Kuo YM. et al. 2013, titled “Exercise benefits brain function: the monoamine connection,” exercise not only improves physical health but also supports brain healing by enhancing neuroplasticity.
- Practice Mindfulness and Meditation: These practices promote relaxation, reduce stress, and enhance self-awareness, which helps break old habits and develop new, healthier responses to stressors.
- Build Healthy Relationships: Surrounding yourself with supportive, sober individuals helps reinforce positive behavior and encourages accountability. Social support strengthens the brain’s reward system and provides emotional resilience during recovery.
- Adopt Healthy Habits: Maintaining a balanced diet, getting enough sleep, and reducing stress are important for optimal brain health.
Proper nutrition and rest allow the brain to heal and function at its best, making it easier to resist cravings and stay sober.
How Do You Get Help for Addiction?
You get help for addiction by seeking professional treatment, support groups, and online resources. The first step in recovery is recognizing the need for help and reaching out to a healthcare provider, therapist, or addiction specialist.
Professional help for addiction offers guidance tailored to your individual needs, helping you navigate the complexities of detox, therapy, and recovery. Support groups, such as Narcotics Anonymous (NA) or Alcoholics Anonymous (AA), provide a sense of community and shared experience, helping you stay accountable and motivated throughout the recovery process.
Many online resources offer educational materials, virtual meetings, and tools to assist you in maintaining sobriety.
What Are the Available Addiction Hotlines and Support Services in the U.S.?
The available addiction hotlines and support services in the U.S. include national helplines and organizations that offer assistance to those struggling with substance use disorders. These services provide free, confidential support and resources for individuals seeking help with addiction.
The available addiction hotlines and support services in the U.S. are as follows:
- SAMHSA National Helpline: The Substance Abuse and Mental Health Services Administration (SAMHSA) offers a 24/7 confidential helpline at 1-800-662-HELP (4357). SAMHSA provides free support for individuals dealing with substance abuse and mental health issues, connecting them with local treatment services, programs, and resources.
- National Helpline for Drug and Alcohol Addiction (NIDA): This helpline is available through the National Institute on Drug Abuse (NIDA) and provides information on treatment options and prevention strategies.
It connects individuals with local recovery support and offers evidence-based information about addiction.
- National Suicide Prevention Lifeline: For individuals experiencing a mental health crisis, including those related to addiction, the National Suicide Prevention Lifeline offers immediate assistance at 1-800-273-8255. While not specific to addiction, it provides necessary support for individuals dealing with co-occurring mental health issues.
- National Alliance on Mental Illness (NAMI): NAMI offers resources and support for individuals dealing with mental illness and addiction.
Their helpline is available at 1-800-950-NAMI (6264) for guidance on mental health challenges and connecting to treatment.
How to Tell If Someone Is Addicted?
To tell if someone is addicted, it’s important to observe specific signs and symptoms that suggest a substance use disorder. Addiction manifests differently depending on the type of substance or behavior involved, but common indicators include changes in behavior, physical appearance, and mental health.
To tell if someone is addicted, the following signs and symptoms are observed:
- Behavioral Changes: Addiction causes noticeable shifts in a person’s behavior. They begin to neglect responsibilities, such as work, school, or family obligations, and engage in risky activities.
You also notice a preoccupation with the substance or behavior, with the person spending increasing amounts of time obtaining or using it. Social withdrawal and a lack of interest in previously enjoyable activities are also common.
- Physical Symptoms: Addiction leads to a variety of physical changes, such as weight fluctuations, poor hygiene, frequent illnesses, and fatigue.
Depending on the substance, there might be specific symptoms, such as red eyes, slurred speech with alcohol addiction, or needle marks in cases of intravenous drug use. Chronic physical complaints, such as headaches or digestive issues, also signal addiction.
- Psychological Signs: Mental and emotional changes also indicate addiction.
This includes increased anxiety, depression, irritability, or mood swings. Individuals with addiction also exhibit paranoia, guilt, or defensiveness when questioned about their habits.
In some cases, people use substances to cope with underlying mental health issues, such as depression or trauma, which worsen the addiction over time.
How Common Is Addiction in the U.S.?
Addiction in the U.S. is a common issue, affecting millions of individuals across various demographics. According to the National Institute on Drug Abuse (NIDA), approximately 19.3 million adults aged 18 or older struggled with a substance use disorder (SUD) in 2020.
In addition to substance addictions, behavioral addictions, such as gambling and internet use, are also prevalent, with estimates suggesting that around 2-3% of the adult population is affected.
Trends show that addiction rates have increased over the past decade, particularly due to the opioid crisis, with opioid-related deaths reaching over 69,000 in 2020 alone. Certain demographics, including young adults, people with mental health disorders, and those living in economically disadvantaged areas, are more vulnerable to developing an addiction.
Share This Post
















